Your rating: None Average: 3 (3 votes)
S. Baboota, R. Khanna, S. P. Agarwal, J. Ali and A. Ahuja
Department of Pharmaceutics, Faculty of Pharmacy,
Jamia Hamdard, (Hamdard University), New Delhi-110062, India.
1. Introduction
A drug delivery system is expected to deliver the required amount of drug to the targeted site for the necessary period of time, both efficiently and precisely. Different carrier materials are being constantly developed to overcome the undesirable properties of drug molecules (Szycher and Kim, 1991). Amongst them cyclodextrins (CDs) have been found as potential candidates because of their ability to alter physical, chemical and biological properties of guest molecules through the formation of inclusion complexes. CDs were discovered approximately 100 years ago and the first patent on CDs and their complexes was registered in 1953 (Loftsson and Brewster, 1996). However, their large scale commercial utilization was prevented mainly due to their high cost and concerns regarding their safety. Recent advancements have resulted in dramatic improvements in CD production, which have lowered their production costs. This has led to the availability of highly purified CDs and CD derivatives which are well suited as pharmaceutical excipients. A lot of work has also been done regarding the safety-assessment CDs and CD derivatives which has allayed the fears which were initially raised regarding their safety. Because of their structure and physico-chemical properties, CDs as drug carriers provide a number of advantages like:
1. They provide a number of potential sites for chemical modification.
2. CDs with different cavity sizes are available which makes it possible to entrap drugs of different molecular dimensions.
3. The microenvironment in their cavity is relatively non-polar and lipophilic.
4. They possess low toxicity and low pharmacological activity.
5. They have a good aqueous solubility.
6. They are rather resistant to hydrolysis by organic acids and many common alpha amylases, and completely resistant to yeast fermentation and beta amylases.
7. They are not decomposed by hot alkali.
8. They exhibit a high thermal stability, with a decomposition temperature approaching 300°C.
9. They protect the included /conjugated drugs from biodegradation.
10. They can be used as process aids to remove specific components from a mixture or minerals.
2. Cyclodextrins and Complexation Phenomenon
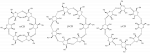
CDs are cyclic (a-1,4)-linked oligosaccharides of a-D-glucopyranose containing a relatively hydrophobic central cavity and hydrophilic outer surface. Owing to the lack of free rotation around the bonds connecting the glucopyranose units, the CDs are not perfectly cylindrical molecules but are toroidal or cone shaped (Loftsson and Brewster, 1996). As a result of their molecular structure and shape, they possess a unique ability to act as molecular containers by entrapping guest molecules in their internal cavity. No covalent bonds are formed or broken during drug-CD complex formation, and in aqueous solution, the complexes readily dissociate and free drug molecules remain in equilibrium with the molecules bound within the CD cavity.
The parent or natural CDs consist of 6, 7 or 8 glucopyranose units and are referred to as alpha (a-), beta (b-) and gamma (g-) CD, respectively. CDs containing nine, ten, eleven, twelve and thirteen glucopyranose units, which are designated as d-, Î-, x-, h- and q- CD, respectively, have also been reported. Hundreds of modified CDs have been prepared and shown to have research applications, but only a few of these derivatives, those containing the hydroxypropyl (HP), methyl (M), and sulfobutylether (SBE) substituents have been commercially used as new pharmaceutical excipients.
3. Advantages of Cyclodextrin Inclusion Complexation
CDs have mainly been used as complexing agents to increase the aqueous solubility of poorly water-soluble drugs and to increase their bioavailability and stability. In addition, CDs have been used to reduce or prevent gastrointestinal or ocular irritation, reduce or eliminate unpleasant smells or tastes, prevent drug-drug or drug-additive interactions, or even to convert oils and liquid drugs into microcrystalline or amorphous powders.
1. Enhancement of Solubility: CDs increase the aqueous solubility of many poorly soluble drugs by forming inclusion complexes with their apolar molecules or functional groups. The resulting complex hides most of the hydrophobic functionality in the interior cavity of the CD while the hydrophilic hydroxyl groups on the external surface remain exposed to the environment. The net effect is that a water soluble CD-drug complex is formed.
2. Enhancement of Bioavailability: When poor bioavailability is due to low solubility, CDs are of extreme value. Preconditions for the absorption of an orally administered drug is its release from the formulation in dissolved form. When drug is complexed with CD, dissolution rate and consequently absorption is enhanced. Reducing the hydrophobicity of drugs by CD complexation also improves their percutaneous or rectal absorption. In addition to improving solubility, CDs also prevent crystallization of active ingredients by complexing individual drug molecules so that they can no longer self-assemble into a crystal lattice.
3. Improvement of Stability: CD complexation is of immense application in improving the chemical, physical and thermal stability of drugs. For an active molecule to degrade upon exposure to oxygen, water, radiation or heat, chemical reactions must take place. When a molecule is entrapped within the CD cavity, it is difficult for the reactants to diffuse into the cavity and react with the protected guest. In the case of thermal or radiation induced degradation, the active must undergo molecular rearrangements. Again, due to the stearic constraints on the guest molecule within the cavity, it is difficult for the entrapped molecule to fragment upon exposure to heat or light or if it does fragment, the fragments do not have the mobility needed to separate and react before a simple recombination takes place. Volatile components can be stabilized against loss by reducing the volatility in case of liquids and by reducing the tendency of some solid products to sublimate. The deliquescence of hygroscopic substances is also reduced by complexation with CDs. Physical changes like sedimentation and caking in suspension or recrystallization of drugs to less soluble but thermodynamically more stable polymorphic crystal forms, etc., can also be prevented or reduced by complexation with CDs.
4. Reduction of Irritation: Drug substances that irritate the stomach, skin or eye can be encapsulated within a CD cavity to reduce their irritancy. Inclusion complexation with CDs reduces the local concentration of the free drug below the irritancy threshold. As the complex gradually dissociates and the free drug is released, it gets absorbed into the body and its local free concentration always remains below levels that might be irritating to the mucosa.
5. Prevention of Incompatibility: Drugs are often incompatible with each other or with other inactive ingredients present in a formulation. Encapsulating one of the incompatible ingredients within a CD molecule stabilizes the formulation by physically separating the components in order to prevent drug-drug or drug-additive interaction.
6. Odor and Taste Masking: Unpleasant Odor and bitter taste of drugs can be masked by complexation with CDs. Molecules or functional groups that cause unpleasant tastes or odors can be hidden from the sensory receptors by encapsulating them within the CD cavity. The resulting complexes have no or little taste or odor and are much more acceptable to the patient.
7. Material Handling Benefits: Substances that are oils/liquids at room temperature can be difficult to handle and formulate into stable solid dosage forms. Complexation with CDs may convert such substances into microcrystalline or amorphous powders which can be conveniently handled and formulated into solid dosage forms by conventional production processes and equipment.
4.0 Applications of Cyclodextrins in Drug Delivery Systems
The multifunctional characteristics of CDs have enabled them to be used in almost every drug delivery system be it oral drug delivery or transdermal drug delivery or ocular drug delivery. The commercial viability of CD-based oral formulations has been established with the marketing of more than 20 products world-wide.
A number of excellent reviews have appeared in the literature in the last few years describing the applications of CDs in various drug delivery systems (Table 1). We present below an update on the recent work done in the different fields.
4.1 Oral Drug Delivery System:
Since time immemorial, out of all the sites available for delivering drugs, oral route has been the most popular route for designing a drug delivery system. In the oral delivery system, the release of the drug is either dissolution controlled, diffusion controlled, osmotically controlled, density controlled or pH-controlled.
CDs have been used as an excipient to transport the drugs through an aqueous medium to the lipophillic absorption surface in the gastro-intestinal tract, i.e., complexation with CDs has been used to enhance the dissolution rate of poorly water-soluble drugs. Hydrophilic CDs have been particularly useful in this regard. Table 2 lists the various drugs that have been evaluated for their ability to form complexes with CDs and the improvement afforded by such complexation.
Rapid dissolving complexes with CDs have also been formulated for buccal and sublingual administration. In this type of drug delivery system, a rapid increase in the systemic drug concentration takes place along with the avoidance of systemic and hepatic first pass metabolism (Jain et al, 2002).
4.2. Rectal Dug Delivery System:
Recent studies have shown that rectal mucosa can be used as a potential site for delivering drugs, which have a bitter and nauseous taste, have a high first-pass metabolism and degrade in the gastro-intestinal pH. It is an ideal route to deliver drugs to the unconscious patients, children and infants. However, rectal mucosa offers a very limited area for drug absorption resulting in an erratic release of drugs. To overcome these problems, a number of excipients have been used and amongst them, CDs have been found to be quite useful.
CDs, to be used as excipient in rectal drug delivery system should have the following characteristics:
1. They should be non-irritating to the rectal mucosa.
2. They should inhibit the reverse diffusion of drugs into the vehicle.
3. They should have a low affinity for the suppository base.
Complexation of hydrophobic drugs with CDs have resulted in a significant increase in the rectal absorption of these drug (Table 3). The reason for the enhanced release has been attributed to the formation of a hydrophilic complex, which has a low affinity for the base and rapidly dissolves in the rectal fluids. It has been reported that the complexation enhances the dissolution of lipophilic drugs at an interface between the molten base and the surrounding fluid and inhibits the reverse diffusion of the drug into the vehicle. Recently the absorption of human chorionic gonadotropin (hCG) was found to increase by about four times in male rabbits when co-administered with a-CD (Kowari et al., 2002)
CDs have also been studied as rectal permeation enhancers. They have been found to increase the permeation of drugs through rectal epithelium cells. It has been reported that complexation of morphine HCl with a and b-CD resulted in an increase in the bioavailability of morphine when it was formulated as a suppository. The complexation increased only the bioavailability and did not alter the release rate of morphine from the vehicle. (Kondo et al, 1996; Uekama et al, 1995) CDs have also been used to prevent the local irritation of drugs on the rectal mucosa.
4.3. Nasal Drug Delivery System:
The use of nasal mucosa for transporting drugs is a novel approach for the systemic delivery of high potency drugs with a low oral bioavailability due to extensive gastro-intestinal breakdown and high hepatic first-pass effect. CDs have the ability to enhance drug delivery through biological barriers without affecting their barrier function, a property which makes CDs ideal penetration enhancers for intranasal drug delivery. CDs can also act as solubilizers for lipophilic water-insoluble drugs, making it possible to formulate such drugs in aqueous nasal spray formulations. Furthermore, CD complexation can stabilize drugs which are chemically unstable in aqueous solutions, and decrease drug irritation after nasal application.
CDs, when used as excipients in nasal drug delivery system should have the following characteristics:
1. They should not have any local or systemic effect.
2. They should not interfere with the nasal muco-ciliary functions.
3. They should not show ciliostatic effect.
4. They should be non-irritating and non-allergenic.
5. They should enhance the permeation of drugs across nasal epithelium in a reversible manner.
The absorption enhancement afforded by CDs can be attributed primarily to their ability to reduce the physical or metabolic barriers to drugs. Another potential barrier to the nasal absorption of drugs is the limitation in the size of hydrophilic pores through which they are thought to pass. The hydrophilic CDs solubilize some specific lipids from biological membrane through the rapid and reversible formation of inclusion complexes, leading to an increase in the membrane permeability. Of all the CDs available, HP-b-CD and methylated b-CDs have been used mainly as solubilizers and absorption enhancers in nasal drug delivery system.
The concept of pulsed estrogen therapy has recently been exploited by the introduction of a nasal spray delivery system containing CD (Al-Azzawi, 2002). The administration of estradiol via the nasal mucosa was made possible by the use of randomly methylated alpha-CD, which increased the solubility of estradiol. The new formulation provided reliable dose-dependent exposure to estradiol, avoiding the hepatic first-pass effect and demonstrated good biological and clinical efficacy. Bioavailability and clinical evaluation of a CD based intranasal formulation of midazolam also showed results comparable to an intravenous formulation with respect to the speed of absorption, serum concentration and clinical sedation effect (Gudmundsdottir, et al., 2001; Loftsson et al., 2001) Table 4 lists the various drugs evaluated for their complexation ability with CDs and incorporated into nasal drug delivery systems.
The safety of CDs as nasal absorption enhancers has also been studied extensively. It has been found that toxicity can occur at two stages. First, when the CD is in direct contact with the nasal mucosa, i.e., local toxicity and secondly, when the CD complex has been absorbed through the nasal epithelium, i.e., systemic toxicity. From the literature review, it has been found that local toxicity of CDs on nasal mucosa is not significant. However, the risk of systemic side effects of CDs after nasal administration depends on how much CD has been absorbed and it has been found that after nasal administration of a drug CD formulation, only the drug is absorbed by the nasal epithelium but not the highly water soluble CD. The CD portion not absorbed is removed by the nasal muco-ciliary clearance system, which transports the unabsorbed CD towards the oesophagus, from where it is swallowed. (Marttin et al., 1997b; Marttin et al., 1998). Asai et al (2002) have recently shown that 30 or 60 min exposure to 10% w/v HP-b-CD or randomly methylated b-CD resulted in no obvious mucosal damage to the nasal mucosa of rats.
4.4. Transdermal Drug Delivery System :
Transdermal drug delivery system is a sophisticated and more reliable means of administering the drug through skin, for local and systemic action. It offers the advantages of minimization of side effects due to the optimization of the concentration profile of drug in blood with time, avoidance of first-pass metabolism, easy termination of therapy by mere removal of patch, predictable and extended duration of action and greater patient compliance due to reduction in the frequency of dosing. However, the most important limitation of this drug delivery system is the limited permeation of drugs through human skin. The human skin is composed of unvascularized epidermis and highly vascularized dermis below it. The external layer of epidermis called stratum corneum is less permeable as compared to the other layers beneath it. Before a topically applied drug can act either locally or systemically, it must penetrate the stratum corneum, the permeation barrier. A number of studies have been carried out to find safe and suitable permeation enhancers to promote subcutaneous absorption of drugs.
Use of CDs as permeation enhancers has gained tremendous popularity over the past few years. The rate of permeation of the drug through the skin is affected by partition coefficient of the drug between the skin and vehicle and the thermodynamic activity of drugs in vehicle.
CDs to be used as excipients in transdermal drug delivery system should possess the following characteristics:
1. They should be therapeutically inert.
2. They should not interfere with the normal functions of the skin such as protection from heat, humidity, radiation and other potential insults.
3. They should not alter the pH of the skin.
4. They should not interact with any component of the skin.
5. They should not cause skin irritation.
In transdermal drug delivery system, hydrophilic, hydrophobic as well as ionizable CDs have been used as carriers for drugs. Hydrophilic CDs like 2,6 dimethyl-b-CD and hydroxypropyl-b-CD have been used to improve the solubility and dissolution characteristics of insoluble drugs. Hydrophobic CDs such as 2,6 diethyl-b-CD have been used to retard the dissolution rate of water soluble drugs and ionizable CDs like carboxymethyl-b-CD, sulfated and sulfobutylether-b-CD have been used to improve inclusion capacity and reduce side effects associated with drugs.
Table 5 lists the drugs which have been complexed with CD successfully in dermal preparation to minimize systemic side effects, improve patient compliance for long term therapy, increase solubility and retard release of drug substances.
4.5. Ocular Drug Delivery System :
In an ocular drug delivery system the most preferred dosage form is the eye drop due to easy instillation in the eye. But the major disadvantage of this dosage form is its inability to sustain high local concentration of drug. The other dosage form for ocular treatment includes oily drops, gels, ointments, suspensions and inserts but these formulations suffer from the drawback of causing irritation and blurred vision. There is therefore a need of an agent, which can overcome these problems while formulating an ocular dosage form. In ocular drug delivery CDs have been used to increase the solubility and/ or stability of drugs and to prevent side effects of drugs such as irritation and discomfort.
CDs have been used to solubilize poorly water soluble drugs and enhance ocular bioavailaibility of lipophillic drugs by keeping the drugs in solution and increasing their availaibility at the surface of the corneal barrier. Hydrophillic CDs such as HP-b-CD and sulphobutyl-b-?CD have been used for the purpose mainly due to their non-toxicity and hydrophilicity. CDs to be used as an excipient in ocular drug delivery system should possess the following characteristics:
1. They should be non-irritating to the ocular surface, as irritation can cause
reflex tearing and blinking resulting in fast washout of instilled drug.
2. They should be non-toxic and well tolerated.
3. They should be inert in nature.
4. They should enhance the permeability of the drug through the corneal mucosa.
Numerous studies have shown that CDs are useful additives in ophthalmic formulations for increasing the aqueous solubility, stability and bioavailability of ophthalmic drugs, and to decrease drug irritation. Table 6 lists the drugs which have been evaluated for their complexation ability and incorporation into ophthalmic drug delivery system.