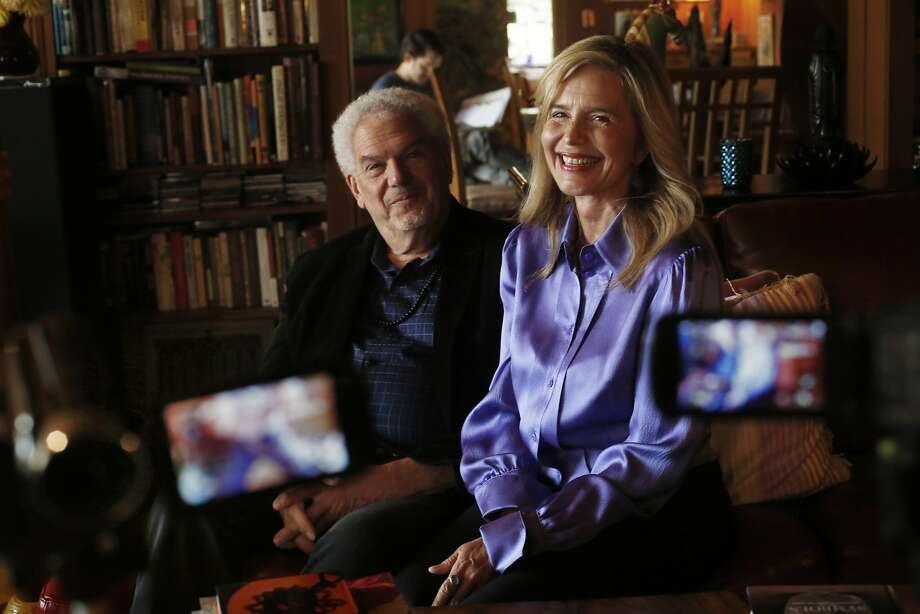
Anne C. Wagner, Rachel E. Liebman, Ann T. Mithoefer, Michael C. Mithoefer, Candice M. Monson
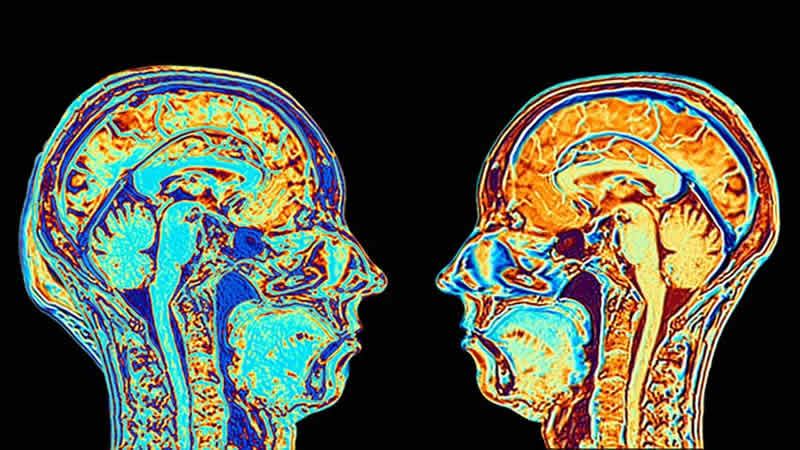
Healing from trauma occurs in a relational context, and the impacts of traumatic experiences that result in post-traumatic stress disorder (PTSD) go beyond the diagnosis itself. To fully understand a treatment for PTSD, understanding its impact on interpersonal, relational, and growth outcomes yields a more fulsome picture of the effects of the treatment. The current paper examines these secondary outcomes of a pilot trial of Cognitive Behavioral Conjoint Therapy (CBCT) for PTSD with MDMA. Six romantic dyads, where one partner had PTSD, undertook a course of treatment combining CBCT for PTSD with two MDMA psychotherapy sessions.
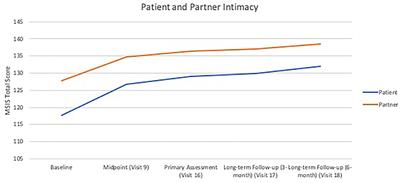
Outcomes were assessed at mid-treatment, post-treatment, and 3- and 6-month follow-up. Both partners reported improvements in post-traumatic growth, relational support, and social intimacy. Partners reported reduced behavioral accommodation and conflict in the relationship, and patients with PTSD reported improved psychosocial functioning and empathic concern. These improvements were maintained throughout the follow-up period. These findings suggest that CBCT for PTSD with MDMA has significant effect on relational and growth outcomes in this pilot sample. Improvements in these domains is central to a holistic recovery from traumatic experiences, and lends support to the utility of treating PTSD dyadically.
Introduction
Traumatic events impact relationships, and healing from trauma occurs in a relational context. Social factors play a key role in the development, worsening, and improvement of post-traumatic stress disorder (PTSD) (
1). Negative social interactions in particular are pernicious in their impact on traumatized individuals, and are associated with higher likelihood of PTSD following a traumatic event (
1,
2). Likewise, the presence of PTSD can have a deleterious effect on relationships (
3), therefore creating a self-perpetuating cycle of exacerbation of symptoms (
4). Given the role of social interactions in the course of, and healing from, PTSD, we examined the relational and growth outcomes in a pilot trial of a dyadic treatment for PTSD, Cognitive Behavioral Conjoint Therapy (CBCT) (
5) for PTSD with MDMA.
Interpersonal functioning, both within and outside of intimate relationships, is often negatively impacted by PTSD, and vice versa. Addressing this impact is important given the fundamental role interpersonal functioning plays in developing and maintaining relationships over time, attachment, parenting, reducing secondary traumatization, and satisfaction and security in life [e.g., (
6,
7)]. Interpersonal traumas more frequently result in PTSD than other forms of trauma in part because of the violation in expectations of relational trust, which then generalizes to other interpersonal connections (
8). Additionally, the content of much trauma-related suffering is interpersonal (including feelings of numbness and detachment from others, cognitive appraisals of trust, control, and intimacy, avoidance of people and situations, anger, and aggression as examples). PTSD can erode relationship quality over time, and conversely, relationships can exacerbate or ameliorate the post-trauma recovery, depending on whether the interactions are positive or negative (
1).
Post-traumatic growth, a construct consisting of relations to others, perceptions of new possibilities in life, perceived personal strength, spiritual change, and an appreciation of life (
9), exists separately from traumatic symptomatology (
10). It is an important outcome due to its reflection of an adaptive cognitive process of adjustment (
11), and is positively associated with resiliency, meaning-making of the traumatic event, relationship functioning and hope (
9,
12). Therefore, post-traumatic growth is indicative of a holistic process of change following a traumatic event.
The loved ones of individuals with PTSD often experience their own struggles in relation to being in relationship with someone who has experienced a significant traumatic event(s) [e.g., (
3)]. This can encompass their own mental health and well-being, quality of life, and their interpersonal relationships and relationship satisfaction with the person with PTSD. While well-meaning, loved ones of individuals with PTSD may engage in behavioral accommodation, a means of trying to ease the symptoms of the person with PTSD (e.g., by reducing noise, limiting the responsibilities of the person with PTSD, excusing aggressive behavior, etc.), which inadvertently may reinforce the presence of these symptoms (
13). Overcoming PTSD ideally occurs in tandem with a greater engagement in life. To foster and support holistic healing, domains related to interpersonal functioning, quality of relationships, and post-traumatic growth need to be considered, as opposed to solely focusing on psychological symptomatology.
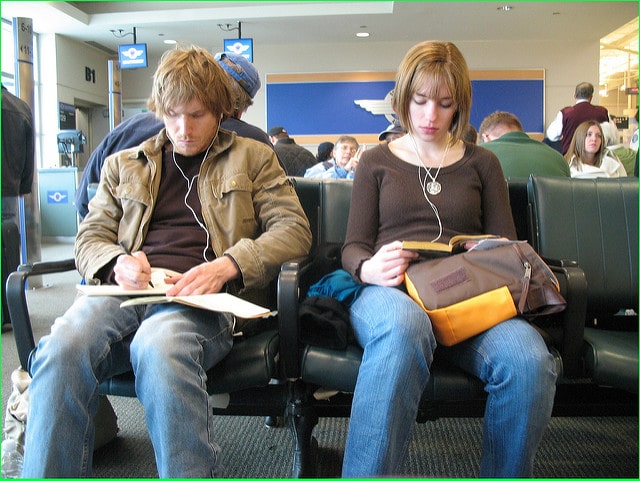
Treating PTSD in a relational framework, and in this case, a couple format, is one means of explicitly utilizing the interpersonal milieu in order to create substantive and lasting change, for both the person with PTSD and their loved one. Cognitive Behavioral Conjoint Therapy for PTSD (
5), a dyadic intervention for PTSD, has shown significant positive impact on both patient and partner mental health and well-being (
14,
15), as well as relational functioning and post-traumatic growth (
16).
MDMA has been used in couple therapy since its first clinical applications in the 1970s (
17–
19). MDMA's empathogenic qualities create a unique therapeutic opportunity in which couples not only feel more comfortable sharing their emotions, but can also approach conversations with greater ease (
20). MDMA has been reported to facilitate individuals' ability to maintain an optimal window of tolerance, allowing for both positive and negative emotions to occur without avoidance or being overwhelmed (
21). This can be particularly useful in addressing couple-based distress and communication.
MDMA-assisted psychotherapy for PTSD has shown promising results as an individual treatment for PTSD in an inner-directed, supportive therapeutic framework [e.g., (
22)]. Participants also report improvements in psychosocial functioning and interpersonal relationships following the treatment, albeit without the use of standardized measures (
23), as well as in post-traumatic growth (
24). Collateral reports of symptoms and outcomes by close others have not yet been collected in MDMA-assisted individual psychotherapy studies, offering an opportunity to expand the understanding of the impacts of the intervention.
We therefore sought to examine patient and partner outcomes related to interpersonal functioning, relationship satisfaction, and post-traumatic growth in a sample of dyads who participated in a pilot study of Cognitive Behavioral Conjoint Therapy for PTSD with MDMA (
25). Primary outcomes from this trial demonstrated significant decreases in PTSD symptoms assessed by independent rater (
d = 2.10), the individual with PTSD (
d = 2.72), and their partner (
d = 1.85) (
25). Treatment gains continued to improve by 6-month follow-up (
d = 2.25, 3.59, 2.72, respectively). The combination of CBCT for PTSD and MDMA was designed to amplify the qualities of each, and in particular, capitalize upon the relational context each is designed for.
Discussion
The couples in this study experienced significant gains in terms of their relational functioning, post-traumatic growth, and behavioral accommodation. They also exhibited gains in or maintenance of strong interpersonal and psychosocial functioning, demonstrating that the combination of CBCT with MDMA for PTSD provides improvements for both partners and the relationship. Additionally, the improvements in minor psychological aggression, and stability of the absence of severe aggression, suggest that the intervention is safe and does not increase a risk of relational or interpersonal harm.
Notably, the improvements in post-traumatic growth were significant for both patients and partners, indicating that both identified growth and change in the partner with PTSD through the course of therapy. Improvements in behavioral accommodation, as assessed by the partner on their own behaviors, demonstrates a greater understanding of the role of accommodation in maintaining PTSD in a relationship, and the choice of the partner to shift their behavior in order to address it.
Improvements in quality of relationship functioning, specifically increases in perception of support and decreases in conflict, demonstrate that this intervention may have promise to strengthen the positive social interactions and diminish the negative social interactions in relationships, both of which are important to recovery post-trauma. Improvements in reported depth of relationship were not significant, which may be partially attributed to the high levels of depth reported by the participants at study baseline. This may speak to couples who are already deeply invested in their relationships as having self-selected into an experimental dyadic treatment for PTSD.
Participants often reported feeling greater connection to others during MDMA-assisted sessions that lasted beyond the therapeutic intervention. Though not formally tested, this experience likely played a role in improvements in intimacy reported in outcome measures. Additionally, improvements in empathic concern and psychosocial functioning for the patient with PTSD suggest a turning toward and engagement with the relationship, and that these results extend beyond the relationship, creating both intra- and interpersonal benefits. This offers a possibility for more holistic improvement and overall well-being. Although partners did not have statistically significant improvement in psychosocial functioning, their baseline scores indicated that they were, as a group, functioning very well, and therefore a large improvement would not have been possible with the intervention. Both partners demonstrated low levels of personal distress related to interpersonal reactivity, potentially accounting for the non-significant findings in this subscale. Patients demonstrated significant improvement in empathic concern, highlighting the relevance of this intervention for improving the well-being of the interpersonal relationship. Partners demonstrated high baseline levels of empathic concern that remained stable over the course of therapy, demonstrating that expressions of empathy can remain stable and improve while engaging in trauma-focused work. Low rates of personal distress and fantasy for both patients and partners were assessed at baseline and remain unchanged.
While the results of the study demonstrate significant improvements, there are numerous limitations to consider. The study sample was very small, and while expected in a proof of concept pilot interventional study, it limits the conclusions that can be drawn. Likewise, the sample was not diverse in terms of ethnicity, race, sexual orientation, and gender identity, suggesting that any conclusions drawn are limited to white, mixed gender, intimate couples. Future studies should place a strong focus on recruiting more diverse and representative samples of participants. The study, by design, was uncontrolled, which means that conclusions regarding the efficacy of the intervention compared to placebo, or either interventional component alone (CBCT or MDMA-assisted psychotherapy), cannot be drawn.
The findings of this pilot study suggest that a larger, controlled study of CBCT + MDMA to explore the relational outcomes of the intervention are warranted. These outcomes also suggest that couple therapy with MDMA may indeed be well-suited for a range of couple-related concerns beyond PTSD, particularly those that are relational in nature. By targeting individual and relational functioning simultaneously, this intervention has the potential to maximize recovery from trauma and enhance present living for those with PTSD and their loved ones.