mr peabody
Bluelight Crew

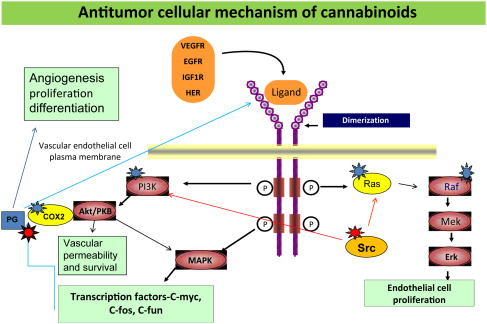
Anti-tumor activity of CBD
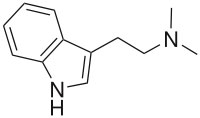
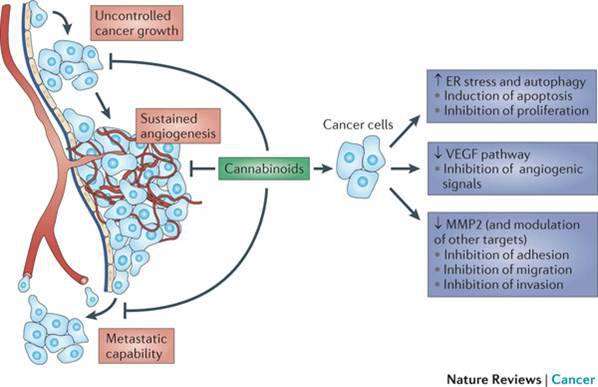
Studies in mice and rats have shown that cannabinoids may inhibit tumor growth by causing cell death, blocking cell growth, and blocking the development of blood vessels needed by tumors to grow. Laboratory and animal studies have shown that cannabinoids may be able to kill cancer cells while protecting normal cells.
A study in mice showed that cannabinoids may protect against inflammation of the colon and may have potential in reducing the risk of colon cancer, and possibly in its treatment.
A laboratory study of delta-9-THC in hepatocellular carcinoma (liver cancer) cells showed that it damaged or killed the cancer cells. The same study of delta-9-THC in mouse models of liver cancer showed that it had antitumor effects. Delta-9-THC has been shown to cause these effects by acting on molecules that may also be found in non-small cell lung cancer cells and breast cancer cells.
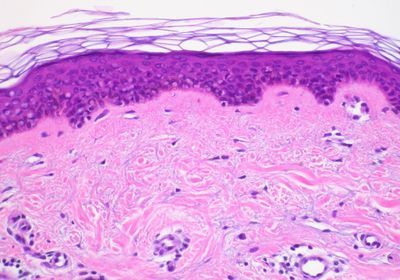
A laboratory study of cannabidiol (CBD) in estrogen receptor positive and estrogen receptor negative breast cancer cells showed that it caused cancer cell death while having little effect on normal breast cells. Studies in mouse models of metastatic breast cancer showed that cannabinoids may lessen the growth, number, and spread of tumors.
A review of 34 studies of cannabinoids in glioma tumor models found that all but one study showed that cannabinoids can kill cancer cells without harming normal cells.
A laboratory study of cannabidiol (CBD) in human glioma cells showed that when given along with chemotherapy, CBD may make chemotherapy more effective and increase cancer cell death without harming normal cells. Studies in mouse models of cancer showed that CBD together with delta-9-THC may make chemotherapy such as temozolomide more effective.
A review of bladder cancer rates in Cannabis users and non-users was done in over 84,000 men who took part in the California Men's Health Study. Over 16 years of follow-up and adjusting for age, race/ethnic group and body mass index (BMI), rates of bladder cancer were found to be 45% lower in Cannabis users than in men who did not report Cannabis use.
A study in mice showed that cannabinoids may protect against inflammation of the colon and may have potential in reducing the risk of colon cancer, and possibly in its treatment.
A laboratory study of delta-9-THC in hepatocellular carcinoma (liver cancer) cells showed that it damaged or killed the cancer cells. The same study of delta-9-THC in mouse models of liver cancer showed that it had antitumor effects. Delta-9-THC has been shown to cause these effects by acting on molecules that may also be found in non-small cell lung cancer cells and breast cancer cells.
A laboratory study of cannabidiol (CBD) in estrogen receptor positive and estrogen receptor negative breast cancer cells showed that it caused cancer cell death while having little effect on normal breast cells. Studies in mouse models of metastatic breast cancer showed that cannabinoids may lessen the growth, number, and spread of tumors.
A review of 34 studies of cannabinoids in glioma tumor models found that all but one study showed that cannabinoids can kill cancer cells without harming normal cells.
A laboratory study of cannabidiol (CBD) in human glioma cells showed that when given along with chemotherapy, CBD may make chemotherapy more effective and increase cancer cell death without harming normal cells. Studies in mouse models of cancer showed that CBD together with delta-9-THC may make chemotherapy such as temozolomide more effective.
A review of bladder cancer rates in Cannabis users and non-users was done in over 84,000 men who took part in the California Men's Health Study. Over 16 years of follow-up and adjusting for age, race/ethnic group and body mass index (BMI), rates of bladder cancer were found to be 45% lower in Cannabis users than in men who did not report Cannabis use.
Cannabis and cannabinoids have been studied in clinical trials for ways to manage side effects of cancer and cancer therapies, including the following:
CBD has been given by mouth to treat solid tumors that have recurred.
An oral spray combining 2 cannabinoids (delta-9-THC and CBD) has been given with temozolomide to treat recurrent glioblastoma multiforme.
CBD has been used to treat acute graft-versus-host disease in patients who have undergone allogeneic hematopoietic stem cell transplantation.
https://www.cancer.gov/about-cancer/treatment/cam/patient/cannabis-pdq#link/_13
Last edited: