checktest
Bluelighter
- Joined
- Jun 9, 2013
- Messages
- 338
Pretty sure most have seen articles correlating dementia and benzodiazepine use, e.g.

 www.bmj.com
www.bmj.com
 www.ncbi.nlm.nih.gov
www.ncbi.nlm.nih.gov
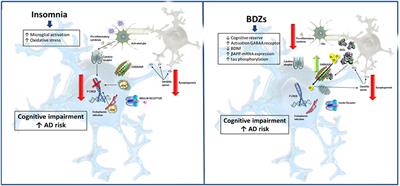
Questions remain of how much is related to the drug vs. indications for taking it (anxiety and insomnia / dementia risks, epilepsy and long-term BZD use, other neuropsychiatric conditions, elements of Alzheimer's, etc...). Cognitive effects and testing vs neurodegeneration. Size of potential actual effect, and so on.
Just curious on thoughts here around the topic, as well as mechanisms related to a possible connection.
Part of this was spurred by this article
 www.frontiersin.org
www.frontiersin.org
Especially the Midazolam Tau hyperphosphorylation mouse study from 2019.
 www.sciencedirect.com
(Which, while finding tau hyperphosphorylation with midazolam notably didn't find major aggregatory changes, though degenerative effects were there. The H(P) persisted past some drug time.)
www.sciencedirect.com
(Which, while finding tau hyperphosphorylation with midazolam notably didn't find major aggregatory changes, though degenerative effects were there. The H(P) persisted past some drug time.)
Hyperphosphorylation of tau (depending on where in tau and the settings) is prevalent in the tauopathies and connected to Alzheimer's, historically as neurofibrillary tangles, with a whole tau hypothesis. Amyloid-beta - tau interactions ("AB as the gun, tau as the bullet").
[Decent open paper showing some of the historical hypotheses for Alzheimer's.
 www.nature.com
]
www.nature.com
]
Neurotrophic effects of benzodiazepines.
Could BZDs interfere with adaptive BDNF responses in some situations? https://pubmed.ncbi.nlm.nih.gov/223...eurotrophic-factor-level-under-mental-stress/
 pubmed.ncbi.nlm.nih.gov
Is it an acute vs. chronic effect?
pubmed.ncbi.nlm.nih.gov
Is it an acute vs. chronic effect?
 journals.plos.org
journals.plos.org
NGF - could there be a cell-type specific interaction or problem with some neurites?
 pubmed.ncbi.nlm.nih.gov
Not sure about GDNF.
pubmed.ncbi.nlm.nih.gov
Not sure about GDNF.
I don't see some excitotoxicity being exacerbated by benzodiazepines, but perhaps homeostasis is thrown off from some circuits being disinhibited or in tolerance to benzodiazepine effects / GABAR distribution.
 www.sciencedirect.com
www.sciencedirect.com
Or perhaps only minor interactions and noise.
Could benzodiazepines exacerbate the course of the dementia, independently of posing as a possible risk factor? Is every old person going to get melatonin drugs and low dose trazodone (or seroquel) instead?
I mean, I don't think benzos are quite like anticholinergics, and there are a lot of issues going on, but sometimes the associations give you a bit of pause. Not a primary risk factor but something to evaluate.
What are your thoughts on benzos and dementia?

Benzodiazepine use and risk of dementia: prospective population based study
Objective To evaluate the association between use of benzodiazepines and incident dementia. Design Prospective, population based study. Setting PAQUID study, France. Participants 1063 men and women (mean age 78.2 years) who were free of dementia and did not start taking benzodiazepines until...
Association between Benzodiazepine Use and Dementia: A Meta-Analysis
The association between long-term benzodiazepine use and risk of dementia remains controversial. Therefore, current study aimed to quantify this association, and to explore a potential dose–response pattern.We searched PubMed, Embase and the Cochrane ...
Questions remain of how much is related to the drug vs. indications for taking it (anxiety and insomnia / dementia risks, epilepsy and long-term BZD use, other neuropsychiatric conditions, elements of Alzheimer's, etc...). Cognitive effects and testing vs neurodegeneration. Size of potential actual effect, and so on.
Just curious on thoughts here around the topic, as well as mechanisms related to a possible connection.
Part of this was spurred by this article
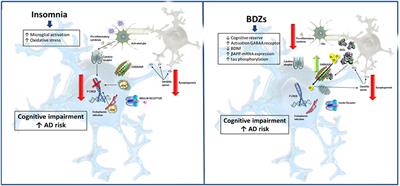
Benzodiazepines and Related Drugs as a Risk Factor in Alzheimer's Disease Dementia
Benzodiazepines (BZDs) and Z-drugs are compounds widely prescribed in medical practice due to their anxiolytic, hypnotic, and muscle relaxant properties. Yet, their chronic use is associated with cases of abuse, dependence, and relapse in many patients. Furthermore, elderly people are...
Especially the Midazolam Tau hyperphosphorylation mouse study from 2019.
Administration of the benzodiazepine midazolam increases tau phosphorylation in the mouse brain
Preclinical studies have shown that anesthesia might accelerate the clinical progression of Alzheimer's disease (AD) and can have an impact on tau pat…
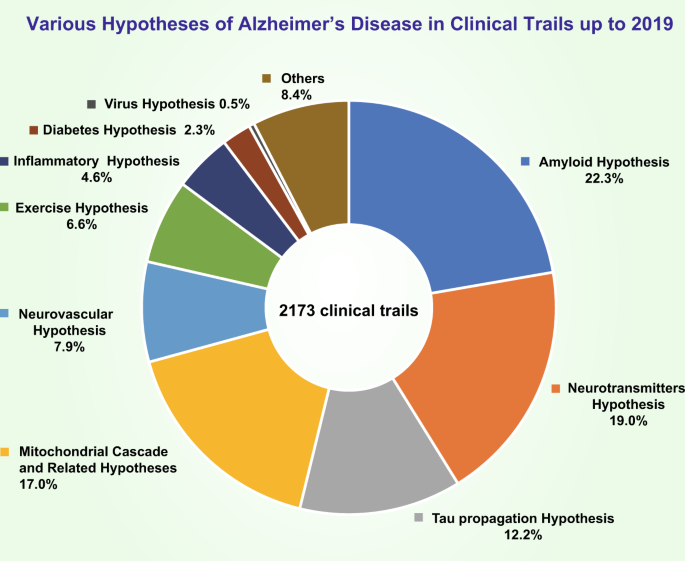
Hyperphosphorylation of tau (depending on where in tau and the settings) is prevalent in the tauopathies and connected to Alzheimer's, historically as neurofibrillary tangles, with a whole tau hypothesis. Amyloid-beta - tau interactions ("AB as the gun, tau as the bullet").
[Decent open paper showing some of the historical hypotheses for Alzheimer's.
History and progress of hypotheses and clinical trials for Alzheimer’s disease - Signal Transduction and Targeted Therapy
Alzheimer’s disease (AD) is a neurodegenerative disease characterized by progressive memory loss along with neuropsychiatric symptoms and a decline in activities of daily life. Its main pathological features are cerebral atrophy, amyloid plaques, and neurofibrillary tangles in the brains of...
Neurotrophic effects of benzodiazepines.
Could BZDs interfere with adaptive BDNF responses in some situations? https://pubmed.ncbi.nlm.nih.gov/223...eurotrophic-factor-level-under-mental-stress/
A Benzodiazepine Impairs the Neurogenic and Behavioural Effects of Fluoxetine in a Rodent Model of Chronic Stress - PubMed
Antidepressant agents such as fluoxetine have been shown to produce neurogenic effects involving transcriptional and translational changes that direct molecular and cellular plasticity. These cellular and molecular events appear necessary to mediate the therapeutic effects of fluoxetine and may...
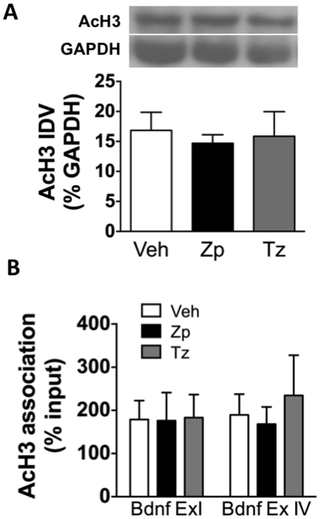
Alterations in Brain-Derived Neurotrophic Factor in the Mouse Hippocampus Following Acute but Not Repeated Benzodiazepine Treatment
Benzodiazepines (BZs) are safe drugs for treating anxiety, sleep, and seizure disorders, but their use also results in unwanted effects including memory impairment, abuse, and dependence. The present study aimed to reveal the molecular mechanisms that may contribute to the effects of BZs in the...
NGF - could there be a cell-type specific interaction or problem with some neurites?
Peripheral-type Benzodiazepines Influence Ornithine Decarboxylase Levels and Neurite Outgrowth in PC12 Cells - PubMed
A number of the benzodiazepines (BZDs) inhibit nerve growth factor (NGF)-induced neurite outgrowth in a dose-dependent manner in PC12 cell cultures. The rank order of potency of a series of BZDs for inhibition of neurite outgrowth does not correlate with the order of their affinity constants for...
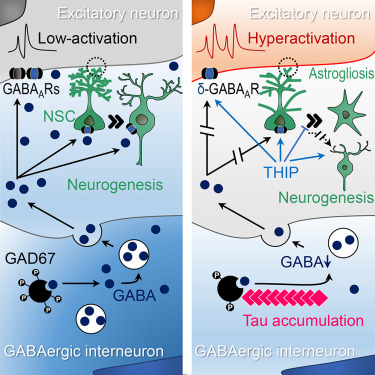
I don't see some excitotoxicity being exacerbated by benzodiazepines, but perhaps homeostasis is thrown off from some circuits being disinhibited or in tolerance to benzodiazepine effects / GABAR distribution.
Interneuron Accumulation of Phosphorylated tau Impairs Adult Hippocampal Neurogenesis by Suppressing GABAergic Transmission
Phospho-tau accumulation and adult hippocampal neurogenesis (AHN) impairment both contribute importantly to the cognitive decline in Alzheimer’s disea…
Or perhaps only minor interactions and noise.
Could benzodiazepines exacerbate the course of the dementia, independently of posing as a possible risk factor? Is every old person going to get melatonin drugs and low dose trazodone (or seroquel) instead?
I mean, I don't think benzos are quite like anticholinergics, and there are a lot of issues going on, but sometimes the associations give you a bit of pause. Not a primary risk factor but something to evaluate.
What are your thoughts on benzos and dementia?

