mr peabody
Bluelight Crew
Benzodiazepine use may increase the risk of Alzheimer’s disease
By Beverly Merz
If you have ever taken Valium, Xanax, or some other benzodiazepine to calm your nerves or sleep better, you may have felt woozy or hungover the next day. Experts have long assumed that people’s heads would clear once they stopped taking the drug. That may not be the case. A study published by the journal BMJ suggests that benzodiazepine use may promote the development of dementia.
A team of researchers from France and Canada linked benzodiazepine use to an increased risk of being diagnosed with Alzheimer’s disease. In the study, the greater a person’s cumulative dose of benzodiazepines, the higher his or her risk of Alzheimer’s.
The association isn’t surprising given past research on the subject, but it still should be viewed with caution. “Benzodiazepines are risky to use in older people because they can cause confusion and slow down mental processes,” says Dr. Anne Fabiny, chief of geriatrics at Harvard-affiliated Cambridge Health Alliance. “However, although there is an association, we still can’t say that benzodiazepines actually cause Alzheimer’s,” she cautions.
Dose, duration, and type of drug matter
The researchers relied on a database maintained by the Quebec health insurance program. From it, they identified nearly 2,000 men and women over age 66 who had been diagnosed with Alzheimer’s disease. They randomly selected more than 7,000 others without Alzheimer’s who were matched for age and sex to those with the disease. Once the groups were set, the researchers looked at the drug prescriptions during the five to six years preceding the Alzheimer’s diagnosis.
People who had taken a benzodiazepine for three months or less had about the same dementia risk as those who had never taken one. Taking the drug for three to six months raised the risk of developing Alzheimer’s by 32%, and taking it for more than six months boosted the risk by 84%.
The type of drug taken also mattered. People who were on a long-acting benzodiazepine like diazepam (Valium) and flurazepam (Dalmane) were at greater risk than those on a short-acting one like triazolam (Halcion), lorazepam (Ativan), alprazolam (Xanax), and temazepam (Restoril).
The researchers acknowledge that the use of benzodiazepines could be just a signal that people are trying to cope with anxiety and sleep disruption—two common symptoms of early Alzheimer’s disease. If that’s true, their use of a benzodiazepine may not be a factor in causing dementia but an indication it is already in progress.
Other reasons to avoid benzodiazepines
Even if that’s so, there are other reasons for older people to avoid benzodiazepines. In 2012, the American Geriatrics Society added benzodiazepines to their list of inappropriate medications for treating insomnia, agitation, or delirium. That decision was made primarily because common side-effects of benzodiazepines—confusion and clouded thinking—often have disastrous consequences, including falls, fractures, and auto accidents.
Even short-acting benzodiazepines pack a bigger punch in older people. As the body’s metabolism slows with age, drugs take longer to clear. And because benzodiazepines are stored in body fat, they can continue to produce effects days after people stop taking them.
Although these medications are taken to help people get a good night’s rest, they can have the opposite effect. “When they’re taken over time, they can actually interfere with normal sleep,” says Dr. Fabiny. The quest to sleep through the night can lead to prescriptions for higher doses or longer-lasting benzodiazepines—and even greater side effects.
If you are a caregiver for an older person, you may want to check the medicine cabinet. If you find benzodiazepine, you might want to discuss it with him or her, or with a doctor.
If you take a benzodiazepine, keep in mind that these drugs are designed for short-term use. If you’ve been using them regularly for more than a few weeks, know that withdrawal symptoms can be powerful. Consider talking to your doctor about alternatives.
There’s currently no cure or treatment for Alzheimer’s disease. That makes prevention all the more important. Limiting the use of a benzodiazepine for anxiety or sleep troubles may be one small step toward prevention.
https://www.health.harvard.edu/blog...ay-raise-risk-alzheimers-disease-201409107397
-----
Deep brain stimulation (DBS) of Alzheimer's patients
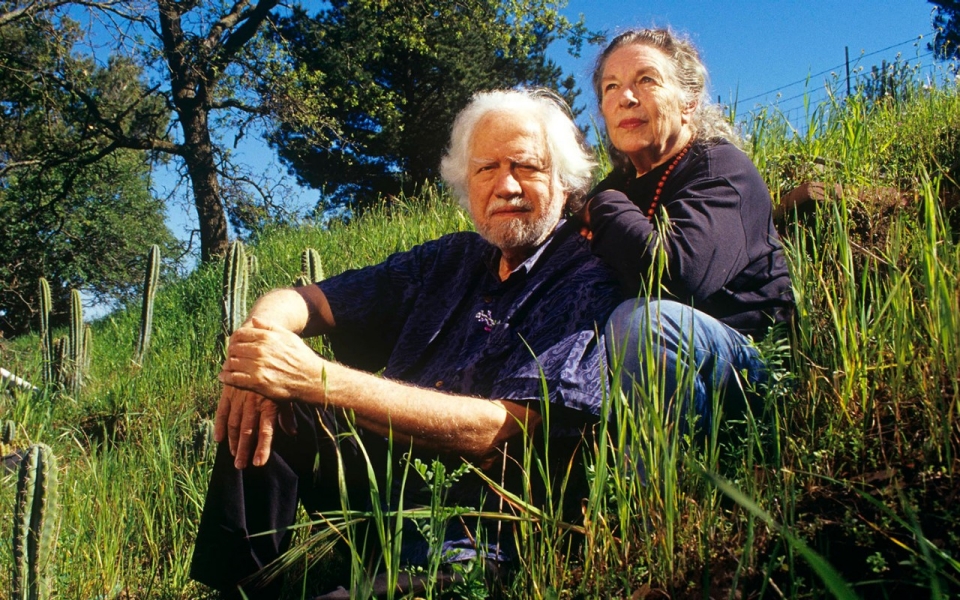
When neuropsychologist Gwenn Smithwas on staff at the University of Toronto, she worked on deep brain stimulation of Alzheimer’s patients with neurosurgeon Andres Lozano.
DBS, in which a medical device is implanted into the brain to stimulate a particular circuit, is used to control tremors in Parkinson’s disease and is under investigation for managing depression
and chronic pain, but its application in Alzheimer’s was novel.
For their pilot, in which DBS was tested in six patients to target the fornix, a bundle of nerve fibers involved in brain memory circuits, Smith analyzed PET scans to study cerebral glucose metabolism to assess safety of the DBS procedure. “Usually, over a 1-year course of Alzheimer’s disease, a decrease in metabolism is observed that correlates with memory getting worse,” Smith explains. Instead, their study observed a sustained increase in glucose metabolism of the brain over one year.
After Smith moved to Johns Hopkins in 2008, she suggested Lozano as the inaugural speaker for the Michael M. Ossoff Visiting Lectureship in Memory Disorders and Alzheimer’s Disease, and introduced Lozano to psychiatrist Constantine Lyketsos. The trio collaborated on a multi-center phase II study of DBS in 42 Alzheimer’s disease patients, further demonstrating safety and a potential benefit for patients over age 65. The study group included an interdisciplinary team of psychiatrists, neurologists, neurosurgeons and neuropsychologists. The work, published last fall in the Journal of Alzheimer’s Disease, was also presented at the Alzheimer’s Association International and Clinical Trials on Alzheimer’s Disease conferences in 2015.
Their study enrolled patients ages 45-85 with mild Alzheimer’s disease. All had caregivers who could reliably report their activities and functioning, and all were taking a stable dose of a cholinesterase inhibitor medication. After the participants were implanted with electrodes, half were randomly assigned to receive continuous stimulation for one year, while the other half received no stimulation. Investigators measured cognitive function and cerebral glucose metabolism.
"Although there were no differences in cognitive outcomes for participants as a whole, in analyses limiting the sample to those 65 and older," says Smith, “there was a trend for cognitive benefit, or even stability, in the older Alzheimer’s patients who were treated with DBS. They showed greater increases in cerebral glucose metabolism, compared with the older patients not treated with DBS. This was not seen in the younger patients.”
Additional analyses of the data are ongoing, some suggesting that stimulation may cause an increase in the volume of the hippocampus, where early Alzheimer’s pathology surfaces.
It’s not clear why younger patients didn’t fare as well. “We hypothesize that an effect in younger patients would be more difficult to detect because both glucose metabolism and cognition decline more rapidly than in older patients,” says Smith. still, “the sense is the treatment is still worth pursuing, but we need to learn more about how to optimize DBS for individual patients, as is well established in Parkinson’s.”
In Parkinson’s disease, clinicians implanting electrodes can determine which contact is more effective by testing the contacts and seeing immediately that if they stimulate in a particular place, tremors stop. In Alzheimer’s disease, explains Smith, it’s not that simple: “We need to develop methods to detect short-term improvement in memory, which is challenging. We also need to learn more about the mechanisms of action of DBS so that we can develop biomarkers to predict treatment response.”
The team is working to define parameters for its next study. Their study enrolled patients ages 45-85 with mild Alzheimer’s disease. All had caregivers who could reliably report their activities and functioning, and all were taking a stable dose of a cholinesterase inhibitor medication. After the participants were implanted with electrodes, half were randomly assigned to receive continuous stimulation for one year, while the other half received no stimulation. Investigators measured cognitive function and cerebral glucose metabolism.
"Although there were no differences in cognitive outcomes for participants as a whole, in analyses limiting the sample to those 65 and older," says Smith, “there was a trend for cognitive benefit, or even stability, in the older Alzheimer’s patients who were treated with DBS. They showed greater increases in cerebral glucose metabolism, compared with the older patients not treated with DBS. This was not seen in the younger patients.”
Additional analyses of the data are ongoing, some suggesting that stimulation may cause an increase in the volume of the hippocampus, where early Alzheimer’s pathology surfaces.
It’s not clear why younger patients didn’t fare as well. “We hypothesize that an effect in younger patients would be more difficult to detect because both glucose metabolism and cognition decline more rapidly than in older patients,” says Smith. Still, “the sense is the treatment is still worth pursuing, but we need to learn more about how to optimize DBS for individual patients, as is well established in Parkinson’s.”
In Parkinson’s disease, clinicians implanting electrodes can determine which contact is more effective by testing the contacts and seeing immediately that if they stimulate in a particular place, tremors stop. "In Alzheimer’s disease," explains Smith, "it’s not that simple: We need to develop methods to detect short-term improvement in memory, which is challenging. We also need to learn more about the mechanisms of action of DBS so that we can develop biomarkers to predict treatment response.”
The team is working to define parameters for its next study.
-hopkinsmedicine.org
-----
Ayahuasca stimulates the birth of new neurons
Studies carried out by the Beckley/Sant Pau Research Program have revealed that ayahuasca use can result in an increase in several key traits associated with mindfulness, such as ‘decentering’, which refers to the ability to observe one’s thoughts and feelings in an objective and non-judgmental way. This, in turn, has been shown to help sufferers of depression, anxiety, grief and PTSD to overcome their conditions.
Brain-imaging studies have revealed how ayahuasca reduces the control of a brain network called the default mode network, and provide compelling evidence that this may be behind the brew’s therapeutic power. Intriguingly, certain compounds in ayahuasca stimulate the birth of new neurons from stem cells in a petri dish. This opens the door to the possibility of using ayahuasca to regenerate damaged brain cells, potentially pointing the way to a new pathway to treating Alzheimer’s and dementia.
-Beckley
Last edited:











