How ibogaine helped me conquer alcoholism
reset.me | 13 Jul 2014
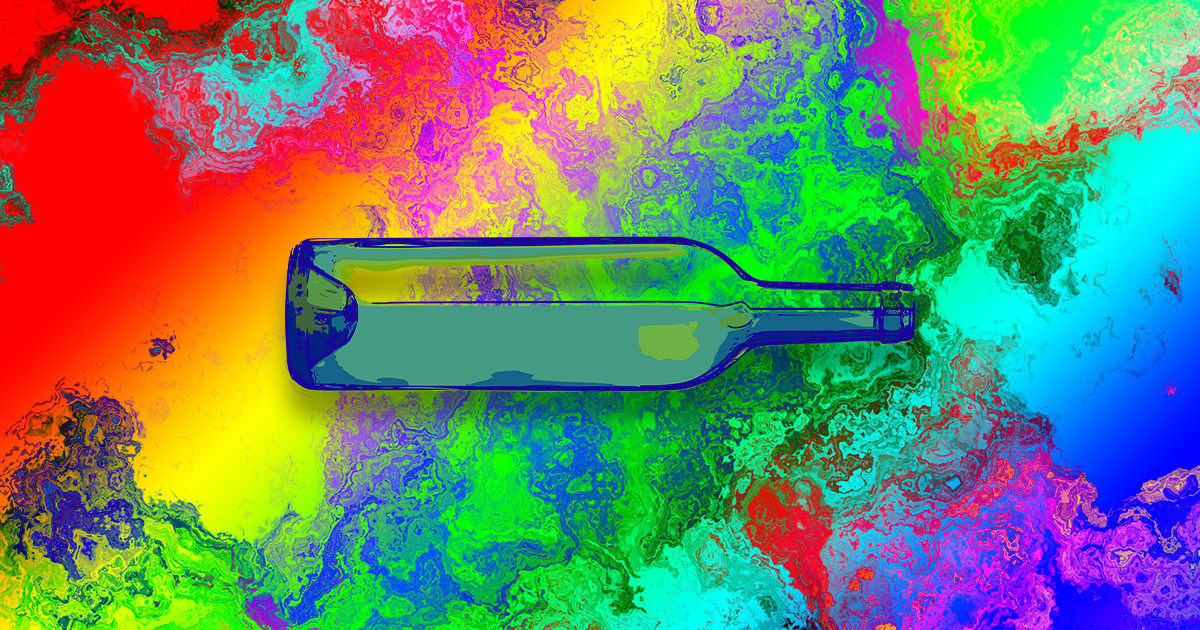
I drank heavily and smoked since I was 18 or 20, taking drugs of all kinds along the way but really seemed to get into the habit of drinking alcohol the most. I live in Milwaukee and went to college here and its socially acceptable to get bombed on the regular and continue with your life. Drinking really is a destination here. So as any of the other drugs I've done fell away due to boredom or lack of skill using them, I just gravitated to the spirits, bad ones, for me anyway. I come from a long line of alcoholics, actually.
I chose a new center that was intrinsically tied to a shaman that came from Africa and has been using Iboga in the Bwiti tradition for a long time. The people that started this place have been training with him for the past number of years to be able to administer and provide an experience that is as comfortable as can be when facing things that aren’t too easy to face. These folks are people with their own stories of abuse and healing. Their own paths to be working with this medicine. And they conduct the ceremonies in a traditional Bwiti way that I didn’t hear about from any of the other centers.
The experience with Iboga is broken into 2 journeys at this center. One is a detox and the other they call a psycho-spiritual journey. The detox varies for everyone and it can last up to 10 days if one is coming off of a heavy heroin diet, or it could be an hour if one is considerably clean. I think.. Now the detox doesn’t just mean a physical detox as Iboga cleans out everything not worth having in you. That being thoughts about oneself that are detrimental, experiences that are harrowing from any age that have stuck to your psyche, bad food, prescription drugs, mental processes etc. It cleans it all out.
As the first journey was the detox Ill start there. We started around the fire and the few providers shared their experiences with how they came to Iboga and came to be working with it. The fire ceremony is important to bring the fire spirits to the area and keep it lit for the duration of the journey. We had a spoonful of raw Iboga root bark that had been ground up all dry and bitter tasting, then chased it with water. That was about 830pm… The time is integral in translating the story just to consider the length of the experience. Then the patriarch of the place spoke of the Bwiti tradition and some of their ways of thinking. Built of tradition and not religion, a way showing, seeing, and experiencing instead of something based on faith. It is something to experience, wholly visceral and tangible. After awhile we were given another bit of Iboga in red pill form that was extract. Then we had more talk of Bwiti tradition.
About what I think was two hours had passed and at this point I was feeling the medicine and decided it was time to go into the temple. The temple is a room made up of 5 single beds spaced about a foot apart and was lit by a few candles around an alter of power objects from Africa. A room in a house actually that is turned into a sacred space safe for traveling. After a quick trip to the bathroom I laid down with my head toward the alter and my feet pointed outside. I was feeling like I had a lead blanket over me like the ones you wear while getting an X-ray and my body was vibrating heavily and tingling with electricity. I can’t remember what my mind was doing… I think I was just noticing how my body felt. A few minutes later one of the providers came over and asked how I was and told me he was going to put some pygmy dust on my 3rd eye with his finger and then he was going to tap on my forehead until I could see his finger. I told him I could perceive his finger but not see it. He told me it was ok and not to worry about it. I then got a blindfold to lay over my eyes because even the candle light was distracting with my eyes closed. As I lay there I started noticing my thoughts and how rapid they were, just blasting to and fro, fast, a bunch of images were moving in front of me but i couldn't seem to grasp them. I’d think
“Oh, that's important, remember that” and as I thought it they would morph into something else and be gone with no memory of what it was. That happened numerous times.
I started feeling like my necklace was constricting me and I needed to take it off, I never take it off and I felt like it just needed it to be off. So I sat up and kept my eyes closed as to not be distracted and undid the clasp and slid it over my head. As I brought it to the front of my face I could see my hands. My hands right in front of me with my eyes closed… and I rotated them back and forth from the palm to the back, to the palm to the back. Just noticing that I could see without opening my eyes. Then I saw my legs, the bed, looking up I saw the pane glass door that was open to the night air, then to my right a fellow journeyman and his bed and bucket. Never had I seen so clear with my 3rd eye. I put my necklace on the floor next to me with a slight cling and laid back down completely astonished.
Now my mind was racing and the images kept coming and morphing and disappearing. I’d shift my position on the mattress and think that I was disturbing the other folks around me, or how I was being perceived laying there. The guy next to me was purging. That was distracting to the point of being pulled out of the trance and I realized I had to pee, so I sat up and motioned for the bathroom. There were 3 providers in the temple that would help with guidance, walking to the bathroom, changing buckets, anything you might need help with in that state of mind. I had to pee so much and I peed almost every time he threw up. The vomiting was almost comforting though. It just felt like… get it out man, get it all out. Then I’d go pee again, probably once an hour during the entire experience. I think it was cleansing my bladder, liver and kidneys from years of boozing. So I’d lay back down and shift and think about how I was disturbing someone, NO ONE was paying attention to my posture or movements to the point of judgement. But I thought they were. That's when I thought… why was I thinking of the way someone else was perceiving me in this state. Everyone was going through their own journey. I did that for a number of hours. Thinking how well I was doing not purging, I was handling the medicine. What a good tripper and traveler I was, look at me. It was all in my mind. I’d been looking for approval and doing things my entire life based on what other people thought of me. Or what I thought other people would think of me if I did. That was a profound thought. I didn’t understand how important that realization was until the next day though it was definitely an “ah ha” moment. Then the thought of how powerful thoughts are came into my mind. How they shape everything around us and our perception of everything around us and how they shape ourselves, and then everything I thought of would materialize.
Part of the Iboga journey is to be able to access yourself, ancestors, and the Iboga plant itself and ask for guidance in answering any questions you have about your life… or anything for that matter. I had thought of a question I’d written down about fear. I've always moved through my life with a lot of fear. Fear of what others will think of me, fear of the unknown, fear of people finding out what I was thinking about myself (which was usually detrimental), fear of failure, success, etc. But I thought of a different question right then instead. I thought
“how can I be a better husband to my wife?” Why that instead of focusing on myself, I don’t know, that's just what happened. Probably because I'm not well adjusted to being able to control my own mind. Just then an image of my wife on a go cart showed up and underneath it the words “trust her” in the font of American currency wrote itself out. I thought
"Wow, ok… why would I not trust her? She’s never done anything for me not to trust her." I then thought about trust and how I've not really trusted many people to the degree of REALLY trusting them. With their opinions, or actions, or whatever. A lot of judgment and stipulation in my trust for others. I then saw images of a million interactions going back to my childhood involving my attitude toward people and how I’d not really trusted. It appeared to me right at that moment I’d never completely trusted myself… and in doing so, never believed in anyone else. Let that resonate… or read it again. I looked as far back as I could trying to find a time when I had trusted myself completely, and couldn’t find a time when I had. My question had morphed into the correct words.
‘When had I started to become fearful’ was re formed into
‘when had I lost my trust.’ I understood that my fear was a by product of such.
I also saw porn images I've watched, sitcoms from the 80’s. For real, I’d find myself in a happy days episode or Mork and Mindy, it was bizarre. Like those shows had programmed something in my young mind about how the world works. I saw old girlfriends, things I was hurt by, and all kinds of stuff that I thought was “lower” in vibration. I thought I was supposed to be having a trip into higher consciousness… I didn’t realize until later after the many hours that passed and into the next day that these were all things that were being taken out of me as a detox.
At dawn one by one we all left the temple for our rooms to be alone and sift through the images and feelings we’d experienced during the journey. Each one of us being escorted by one of the providers that had been in the temple with us through the night. Back in my room I cried like Ive never cried before. And because I was ready to heal and just surrendered I just let it come. I probably cried and sobbed for about 2-3 hours on and off. Every time I felt like I had to cry I just cried. I let it all out. Now some of you may be used to crying and I thought I was. I cry at the beauty of a song that touches me or a movie that's done right. Or at my son and his accomplishments or failures, and maybe just how beautiful things are to him. I usually hold back though and defer it to some other time, which never comes. So I just let it go. There weren’t really any thoughts tied to it besides how I've treated myself and my family over the years. Nothing ridiculously horrible, just embarrassing or bad to me. Things I’d missed from being hungover or being drunk at inappropriate times or things I’d said. HA, so I guess it wasn’t nothing...
The providers would come and check on us about every hour, bring us fruit and make sure we had water. Granted I wasn’t able to eat anything until 9 or 10 the next evening. The time line was pretty harrowing as I said before. Ceremony started at 7:30, medicine was ingested around 8:30, go into temple I guess around 9:30 or 10. At dawn we’d go to the rooms and sleep wouldn’t come until around midnight the next night. So that puts it at about 30 hours of introspection. They say Iboga will let you sleep when its done working on you. But I was so tired and drained from the experience that I’d just lay there awake remembering and trying to write or record my voice with some of the things that happened.
After some sleep we had a day of rest and were taken to some hot springs for a mud bath and a swim. Some delicious organic food was served up and we met other folks from a similar Iboga center and talked with them and each other about our experience. Everyone's experience was just as different than the next. The similarities seemed to be only in the “ah ha” moments.
Sunday was the next ceremony and it started the same way with all of us around the fire and a few people shared some things, then they asked us to share some things from our first journey. I think a lot of folks felt like it was really almost too personal. Or maybe they hadn’t processed some of the heavier stuff that they saw or felt during. I offered up the 2 major things that I didn’t think were too personal to share and vocalized about how I feel like I’d been doing things for approval for most of my life instead of doing things for myself. And not trusting myself for however long. We also had our questions written down for the guided part of the journey if we ever got there. Later in the week the doctor that lives there stated that people spend 10 years to come to conclusions like that and it happened in one night. He said he didn’t know how Iboga does it, but it does. He has seen it over and over. Besides being there for any health concerns he is studying the effects of Iboga for these reasons.
We also did a few other things that I’ll leave out. If you choose to have the experience you can see for yourself. This time the medicine started to hit me early and I figured it was time to go into temple and lay down. As I lay down, one of the providers gave me the blindfold for my eyes. I lay there and put my hands directly across from each other over my chest. I could feel the electricity between them and sort of played with it for a bit. Its an amazing feeling to play with the energy, its like two magnets pushing against each other. I was in awe of that and could feel my body just vibrating like crazy, like I was plugged in. I've had other psychedelic experiences and it was quite similar with the onset. Granted it wasn’t a nervous feeling like the onset of acid or mushrooms can be. But having a psychedelic reference point was nice. I started to spin round n round like the alcohol spins and I opened my eyes and said stop, and the spinning stopped… then closed my eyes and it started up again. But then the spins shifted and I felt like I was spinning flat on top of a figure eight like the infinity symbol but it was just my head and feet dipping instead of a full out spin.
The medicine started to really come on and I wasn’t sure what to expect. I was trying to have no expectations but it was really coming on and I wasn’t sure what was happening. My body just kept vibrating at a higher level minute by minute and it wasn’t topping off, the medicine was kicking. So I felt an intuition and voice inside me say “go”. Then I said to myself
“I’ll let the medicine come on stronger,” then again,
"Go, no I’ll wait, I should go, no I’ll wait." I was really afraid but I didn’t know of what and I wasn’t sure of where I was gonna go? I was just staring into black space. I was really fighting with myself and maybe it was just to let go… or to actually go somewhere. All I know is what happened next is one of the most poignant and helpful things I’ve ever felt when it comes to having support from friends and family. Out of my pillow from under my head my sons face showed up in all its two front toothless glory and whispered into my ear…
”Just go daddy” I’m tearing up as I write this.
“Just go.” Then behind my son my wife shows up and she puts her arms around him, and she says
“This is why you came down here, you should go.” And what did I say?! I’ll wait till the medicine kicks in a bit more!!!!! Gsus! There was something blocking my view off to the left like a black object… I couldn’t see past it and that was the way I wanted to go or where I was being pulled toward. I then saw two really good friends Dustin and Kristine in the sky off in space. I asked them ..
"Is it clear over there?” Dustin goes,
“Yeah, it's clear, you can go.” Kristine was patting her thighs and clapping encouragingly saying
“Yeah, go, go” and Dustin is saying “gooooo” like he’s calling me onto a wave..this one’s yours man I can see it, go go go, like paddle man, you got this. My wife is saying Go and my boy is saying Go. In this cacophonous sound of 5 people coming to a crescendo of GO! I couldn't deny it anymore. My body was just really moving, like my spirit was about to come out of it. I raised my arm like I was in school or something and said to one of the providers…
”Hey, I need some guidance over here..." He asked what was going on and I said
“I’m being told I need to go,” and he says,
“Where do you need to go?” Like he was wondering hmmm, what's he wanting, does he feel he needs to leave the temple or something?… not sure. I was lucid enough to tell him ..
”Oh shit, I’m not explaining myself correctly,” and told him the scene that was happening as we were speaking with everyone telling me to go. He said
“Alright, let’s do it.” I don’t remember if that's exactly what he said, but it was similar in resonance.
He guided me to my house and told me to go inside. Remember that I said in this state anything I thought of would materialize? Literally anything that came into my mind would appear. I went inside the front door of my house and stood in my living room. He asked if anyone was there and I panned the room with my eye. In the dining room… it was me. I was standing face to face with myself.
Many things happened during this part of the journey and Im not going to go into it here but it was extraordinary in every aspect. I dealt with so many things that have hampered me in my past. I had questions written out that the provider read to me and I would repeat them aloud getting answers immediately from myself. You can ask anything and most of my questions were very personal in nature about events and people in my life past and present. And for the first time in my life things were clear about where I’d come from, who I am, and my place in all of it.
At one point I started breathing really heavily and the vibration of my body was extreme, just total surrender…and it was buzzing. I started breathing hard enough and I was not focusing on the questions at hand. Later a guy in the ceremony said he had sat up thinking something may have been wrong. The provider asked me what was going on. I said if I have to fly again I’m flying with my soul. He asked me what I was doing and I said I was flying with my soul into space and a very high speed, holding onto his ankle. I mean we were moving! Just sonic. He said
"Well you can fly all night maybe you can ask him to come back so we can get to some of these questions answered." I had a full page written out. Kinda funny actually. We came back down to earth and sat back down on some stairs of a deck where we were talking.
Like I said I'm not going into the main answers I received because if you want it, you can have your own experience. But I’ll tell you this, it was the most spiritual experience of my life. And I've had a few in my life but they were nothing like this. I got access to the spirit world and spent a number of hours there traveling and reconnecting with my spirit guide and soul. And I was the bumbling fella trailing behind trying to keep up with them both. I remember yelling to my soul as they walked up a hillside
“Where are you going?” He said
”As long as he’s around I’m hanging with him.”
After a brief exchange about going around with each other into the ether, we took off on a chalkboard eraser in to the spirit world to see some things I was to be shown. At this point in the journey had become extraordinarily psychedelic and it was all I could do to stay focused and ride around on the vehicle which we chose to use. I would get distracted by something the Bwiti music would be building in the trip and I would go into it and become part of it. After I don’t know how long I would think to myself…
”I was doing something…not sure what but I was focusing..” I’d hear a whistle and look up, and there would be my soul and my guide on the eraser and they’d motion for me with an arm wave saying c’mon let's go. With no judgement I’d be back in the front seat and we be trucking along looking at the nature of reincarnation, the fate of the earth, my birth, and questions I hadn’t even thought of. Every time I’d get lost in the trip I’d do the same thing. My guide and I worked out a meeting place after a few times of just coming to and having them whistle. I would picture a kid's slide, one of those spiral slides at a playground. It was blue with a yellow top. I’d come to, out of some psychedelic mechanism remembering I was doing something and in an instant, I’d run up that slide under the hood of yellow and hop into the eraser and we’d set off again into the ether. A generalized meeting place that would appear just as I thought of it.
I do apologize I can’t divulge all of this part of the journey because I know I would want to hear it from someone after all the stuff from the detox. But it was such a beautiful experience reuniting with myself and my guide that its just that close to my heart that I don’t want to put it all out there. We all have these things in us that are just for us.
It is very soothing to have some clarity on the things that have tripped me up for so long. Some perspective that I had not know previously. It's like all of the things I learned were already things I knew but couldn’t access until I let go fully and surrendered. I can’t emphasize enough the amount of surrender it took to just let all this information come. I know some folks fight this stuff and that's gotta be harder than just letting it happen. I was ready to heal and let whatever information come through that was going to, the good, the bad and the ugly, accept and let it go. It wasn’t pleasant seeing and reliving certain things from my past, but it was awe inspiring.
I could’ve written a novel considering the amount of things I experienced during the journeys and during the 8 days I was there. Granted if I had better grammatical knowledge I probably would. And this was just a small portion of all the pageantry and fireworks that an Iboga experience can bring. As I sit here on my porch with the mid-western summer rain coming down in buckets and my son sound asleep in bed I feel extremely grateful. Grateful for the man I once was that pushed to seek answers and healing. And the man I am now, continuing to work on myself in so many ways. I was, as Mike Ness’s album title describes, ‘cheating at solitaire’ and it was wholly unfair to myself. It seems to me that the medicine called to me. Or I was drawn to it. Whichever the case, Iboga is what provided the catalyst to change for me. It helped me get out of a pattern of bad thoughts, horrible actions, and negative vibrations mostly focused toward myself. It's not a magic pill, it doesn’t do the work for you. It seems to open a doorway to walk through. But the work has to be done continually, it just seems clearer now as to what I have to do for myself to sustain a healthy and happy life.
The lessons have stayed with me for the most part though the novelty of the experience has faded. I'm watching my thoughts more clearly, I am grateful every morning for the day prior, and the day to come, and I conquered my alcoholism and the hounding of that demon.
I stand taller, breath deeper, and feel calmer.
I am grateful.
http://reset.me/personal-story/personal-story-healing-ibogaine/