mr peabody
Bluelight Crew
- Joined
- Aug 31, 2016
- Messages
- 5,714

Using psychedelics to heal from sexual trauma
by Sophie Saint Thomas | DoubleBlind | 29 Jan 2020
Psychedelics are promising tools to help survivors reprocess their experience and heal from PTSD.
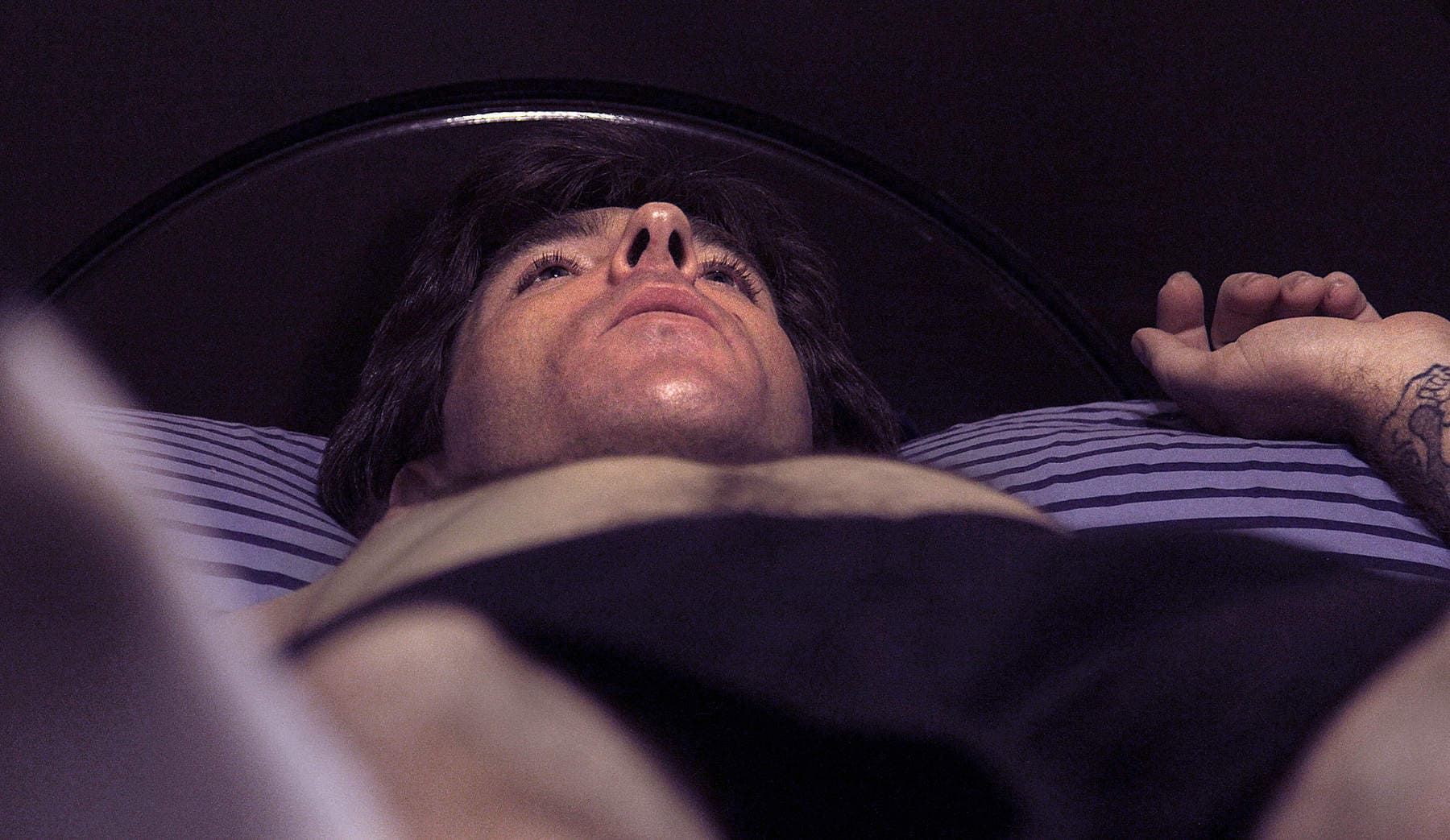
Psychiatrists diagnosed me with so many different conditions after I was sexually assaulted that I don’t remember them all. What was wrong with me? Suggestions included generalized anxiety disorder, insomnia, ADD, panic disorder, and depression. It turned out that I had PTSD, which is an insidious monster with many arms that do indeed manifest as everything from insomnia to flashbacks to depression. What I really wish is that someone had told me: “You were raped. That's awful, and life is going to be a bit harder now. But you are strong, and you will be okay.”
While I took SSRIs and went to therapy, my first memory of real healing was through cannabis. It took away nasty flashbacks getting in the way of my sex life. But while cannabis currently may be the most mainstream medicine in the psychedelic community, it’s far from the only one helping sexual assault survivors heal from trauma.
“I think that psychedelics can be used as tools to help people access greater embodiment and safety around reprocessing their trauma and, in the words of sex therapist and psychedelic integration therapist Dee Dee Goldpaugh, experiencing a ‘compassionate recasting’ of ourselves in the story,” says activist Leia Friedman, host of The Psychedologist: Consciousness Positive Radio. “MDMA is probably the most commonly used medicine for treating sexual trauma, but I have heard from different people that ayahuasca, psilocybin, ketamine, LSD, and mescaline-containing cacti were all helpful, as well.”
Years after my assault, when that asshole, depression—a side effect of PTSD—showed up again, I began Ketamine intravenous therapy, which has been shown to help both PTSD and treatment-resistant depression. It worked better than anything I had ever tried.
For those like Alexandra Evers, 30, psilocybin intervened. The Detroit-based graphic designer had been in an emotionally, physically, sexually and financially abusive relationship for six years. Against her abuser’s wishes and behind his back, she took shrooms with her best friend. “It was a transformative experience for me, and I believe I would be dead today if I hadn’t gone through with it,” Evers says of that first trip. “I was able to step outside of myself. I saw my life from a wholly different point of view that my inhibitions and denial hadn’t allowed me to see.” Later, alone in her apartment, a realization hit Evers: “I was suddenly overcome with the knowledge that he would kill me. It was a shining moment of perfect clarity that I had never experienced before and haven’t since. I knew that he would murder me if I didn’t pack up and leave. So I left.”
Evers’ experience demonstrates the unique power of psychedelics to provide a lightning bolt of realization. “Psychedelics like mushrooms help you access a shift in self-consciousness,” says Michelle Janikian, author of Your Psilocybin Mushroom Companion: An Informative, Easy-to-Use Guide to Understanding Magic Mushrooms. Evers survived the abusive relationship she was in, but her departure from it was not uneventful. “Two months later my abuser shot himself in the head with a shotgun in that apartment,” she says. “I know that if I had been there, he would have killed me too. I am absolutely sure of it.” Today, Evers continues to use psilocybin on her own with people she trusts to guide her through working on her trauma.
Perhaps a reaction to such a cruel violation, perhaps because survivors who come forward are often called liars, but it’s beyond normal to blame yourself after sexual assault or abuse. Psychedelics, however, may be uniquely poised to treat PTSD stemming from sexual abuse because they help the survivor step outside their traumatized minds and see themselves compassionately. Ketamine works behind the scenes, restoring structure and anatomy, stimulating the dendritic and synaptic growth that was disrupted through childhood trauma. You experience relief about ten hours after the IV infusion (in my experience, a dissociative high is mostly a pleasant side effect), other medicines treat trauma through the trip itself.
“Using the psychedelic psilocybin and the empathogen MDMA can both create psychic spaces within individuals to gain a deeper sense of self,” says psychologist and sexologist Dr. Denise Renye. “MDMA can help an individual recollect a sexual assault without the PTSD symptoms of freeze, flight or flight. MDMA can also allow for the survivor to have a sense of empathy for their self that went through the assault, thus alleviating some of the self-judgement that sometimes accompanies it.”
Research shows that PTSD causes changes in the hippocampus, amygdala, and medial prefrontal cortex, which leads to alterations in memory. Psychedelics can help survivors see their experience the same way we’d view an assault that happened to our best friend—with compassion rather than self-blame.
Of course, there is one glaring, deplorable elephant in the room: Most psychedelics are illegal. While this doesn’t prevent survivors from obtaining them, it does make it tricky to do so in conjunction with therapy. “Integration is greatly important. This can be done with a therapist who understands the healing potential of plant medicines and empathogens,” Renye says.
Integration, as the name suggests, refers to integrating wisdom learned from a psychedelic experience into your day-to-day life. It’s wonderful to feel deeply compassionate to yourself during a trip, but speaking therapeutically, it doesn’t matter much if that feeling isn’t harnessed, nor those lessons maintained. “If proper integration is not done mindfully, it will just be a trip and the journey aspect of it will be lost,” Renye says. “It is a journey from feeling broken to experiencing one’s self as whole.” Proper integration, she adds, can be done with a therapist one-on-one, or in a group setting.
"Integration is an ongoing process that may include meditation, conscious body movement, mindful walking in nature, and sound healing," Renye says. She also recommends keeping a journal after the journey, as it might be easy to forget the transformations that occurred.
Cities such as Oakland and Denver are decriminalizing psilocybin, and researchers are conducting trials on MDMA, ketamine, and more for PTSD treatment. The future looks hopeful but we—survivors of sexual assault—have a long road ahead of us. For now, if you’re a survivor considering psychedelics, remember how important setting and integration are. “I do not advise recreational use for the purposes of healing a sexual trauma,” Renye says. “I also do not advise doing this sort of experience without the guidance of someone who is trusted and trained. If set and setting are not taken into consideration, there is potential for a deeper level of trauma to occur.”
At the very least, it’s a good idea to have a trusted friend with you to act as a “sitter.” “Before the journey, talk with the sitter about ways to ask for support, such as physical contact like a hand to hold or a shoulder to lean on,” says Leia Friedman. “It’s important to also discuss how to stop physical contact both verbally and non-verbally, and both people must agree that there will be no sexual contact during the session.” Some professionals warn against using psychedelics for trauma without the aid of a trained therapist, because there is a risk of opening old wounds.
I can’t emphasize enough the relief I felt after I found ketamine. It was as if I had been swimming in choppy waters (and acting like it) and suddenly I could stand calmly on land. “How the hell, did I not know this option existed earlier?” I thought over and over. I continued to see a therapist and take my SSRIs, but psychedelic medicine provided a massive change. If you’re a survivor reading this story, until you find your medicine, let me remind you: It’s not your fault.

Using Psychedelics to Heal from Sexual Trauma | DoubleBlind
Sophie Saint Thomas used ketamine to heal the trauma of rape; other survivors of sexual assault have also turned to psychedelics. Read more at DoubleBlind.