I found all this very interesting and it pertains to the increasing use of ketamine as an antidepressant. I think it’ll be best to cut quotes and talk on them intermittently. They say it a lot better than I will..
“The ‘gut-brain axis’ represents a complex network of pathways interconnecting the gut and the brain, comprising the central nervous system (CNS), the sympathetic and parasympathetic branches of the autonomic nervous system (ANS), the enteric nervous system (ENS), as well as the wide array of cells in the gastrointestinal microenvironment.”
“An exciting emerging issue is that the extension of this microbial influence to the CNS may contribute to the regulation of brain development and behaviour.”
“Tryptophan is an aromatic amino acid containing an indolic group attached to an alanyl side chain. The aminoacid is essential for animals and humans, which prevalently derive it from exogenous sources, such as dietary nutrient intake, and, only in part, from endogenous protein degradation. The main dietary sources of tryptophan are chocolate, cereals milk, milk derivates, red meat, poultry, eggs, fish, and dried fruits.”
“In the gut, the amino acid may be also metabolized, under direct or indirect control by the microbiota, giving origin to several compounds, such as 5-HT, kynurenines, tryptamine, and indolic compounds, which participate in the microbiota-gut-brain communication.”
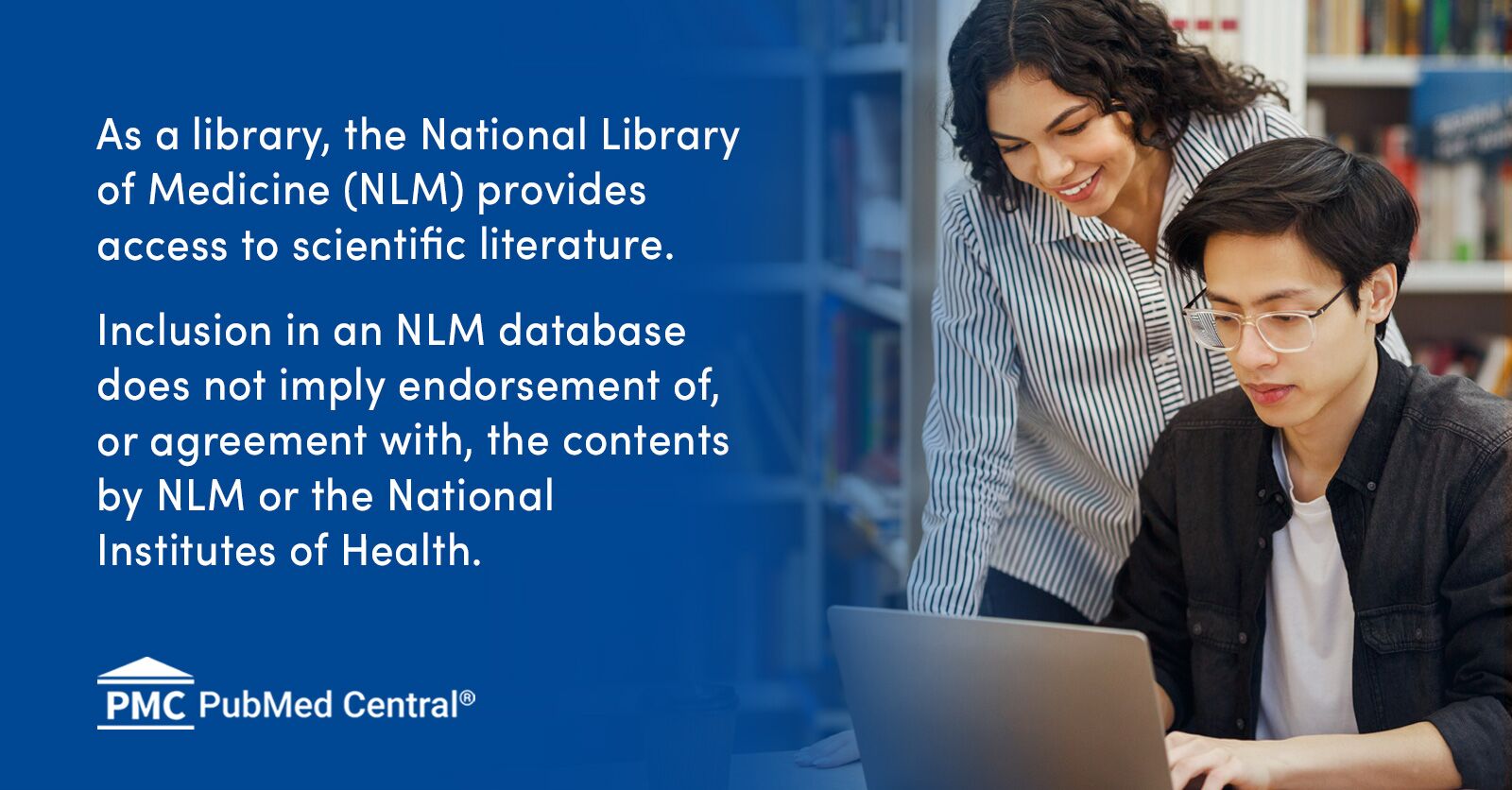
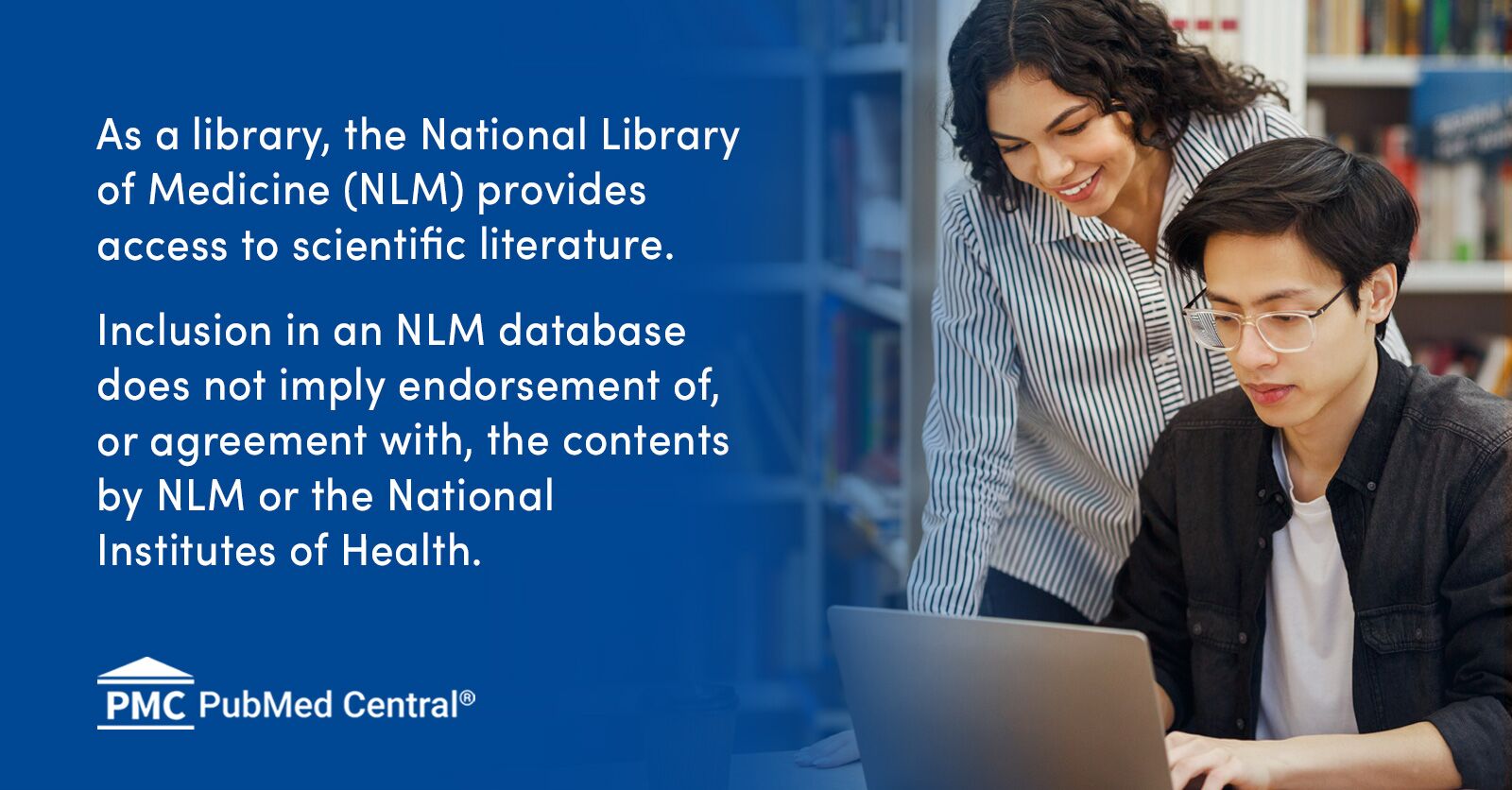
“Under normal conditions, about 90% of the assumed tryptophan is catabolized and transformed into kynurenine through the kynurenine pathway, while approximately 3% is metabolized into 5-HT, and the remaining is degraded by the gut microbiota to produce indole and its derivatives.”
“…metabolites of the kynurenine pathway, collectively called kynurenines, in particular quinolinic acid and kynurenic acid, may influence neuronal activity both in the CNS and in the periphery, retaining neurotoxic and neuroprotective properties, respectively. In this perspective, an unbalanced kynurenine metabolism has been suggested to underlay development of microbiota-gut-brain axis disorders.”
“Quinolinic acid may act as an excitotoxin both in the peripheral and CNS, due to its agonist properties at ionotropic glutamatergic N-methyl-d-aspartate (NMDA) receptors. Quinolinic acid increases extracellular glutamate levels and acts synergistically with the amino acid to induce NMDA-mediated excitotoxicity.”
“A growing body of evidence suggests that quinolinic acid may participate in the pathophysiology of several psychiatric and neurodegenerative disorders. In contrast, kynurenic acid is considered to be neuroprotective, acting as an antagonist at NMDA receptors both in the CNS and in the ENS.”
“Both in IBS and IBD, changes in the microbial community and in its metabolites participate in dysfunctions of the epithelial, immune, and neuronal gut compartments. It is now assessed that such derangements may not only underlay gut symptoms but may also influence the gut-brain communication, predisposing to CNS disorders. In this scenario, impaired tryptophan metabolism along the microbiota-gut-brain axis may potentially participate in the manifestation of both local and CNS symptoms associated with both diseases.”
“IBS patients may frequently experience high levels of anxiety and depression with respect to healthy subjects, regardless of the IBS subtype. Both psychiatric disorders are closely related to stress, an important pathogenic factor for IBS.”
“From a metabolomic stand point, changes in microbiota composition during chronic stress is associated with the diversion of tryptophan metabolism from the 5-HT to the kynurenine pathway. Administration of the probiotic Lactobacillus reuteri in mice subjected to stress stimuli attenuated the unbalanced tryptophan transformation, reinforcing the concept that the microbiota may influence metabolism and resilience during stress.”
“Interestingly, anxiety-like behaviours developed in mice receiving gut microbiota from depressed patients in parallel with increased blood kynurenine levels and kynurenine/tryptophan ratio.”
“Manifestation of depressive symptoms in IBS patients was correlated with altered tryptophan metabolism.”
“Kynurenine involvement in stress-related disorders may depend on the ability of this molecular pathway to influence NMDA receptors located in CNS regions involved in the development of depression, such as hippocampus, amygdala, and cingulate cortex.”
“In mice, the prodrug, 4-chloro-kynurenic acid, induced a rapid onset of antidepressant effects, displaying a better safety profile than other glutamatergic antagonists already used in clinical settings, such as ketamine, holding promises for use in humans.”
“In the gut, the modulation of the kynurenine pathway in favour of kynurenic acid synthesis may be neuroprotective to compensate for inflammation-induced increased NMDA receptor activity in the neuromuscular compartment.”
“Quinolinic, as a neurotoxic NMDA agonist, has been suggested to participate to depression development. Data from clinical investigations suggest that kynurenic acid/quinolinic acid ratio may represent an index of neuroprotection, and a reduced ratio may be indicative of inflammation-induced depressive disorders.”
 www.ncbi.nlm.nih.gov
www.ncbi.nlm.nih.gov
“Quinolinic acid…is often implicated in the pathogenesis of a variety of human neurological diseases. QUIN is an agonist of N-methyl-D-aspartate (NMDA) receptor, and it has a high in vivo potency as an excitotoxin.”
“Free radical generation and oxidative stress are involved in the QUIN-induced toxicity; however, we need to take in mind that these mechanisms can be dependent and/or independent of its activity on NMDA receptors. In this line, it has been shown that QUIN can produce oxidative damage independent of its activity under NMDA receptor; this mechanism involves a complex between QUIN and Fe2+.”
“Inflammatory events are also implicated in the QUIN toxicity. It is known that microglia is responsible for inflammatory responses in the CNS and takes the major role in altered levels of QUIN…”
“…large amounts of QUIN are produced and secreted by activated microglia. During CNS inflammation, QUIN levels increase in brain homogenate (246-fold) and extracellular fluid (66-fold).”
“Several reports have been shown that the intrastriatal administration of QUIN in rats produced significant behavioral changes.”
“On the other hand, the few studies in which it has been investigated the cognitive deficits of rats with QUIN lesions have indicated that this metabolite causes deficits in spatial reference memory.”
“Alteration in QUIN levels has been implicated in different pathologies such as Alzheimer's, Huntington's, and Parkinson's diseases..”
 www.ncbi.nlm.nih.gov
www.ncbi.nlm.nih.gov
GC- Alright that’s enough quotes for a minute. In a nutshell what are these two articles saying?..
The serotonin that our bodies need to function at homeostasis is derived from tryptophan which is more or less produce by microbes in our gut.
With an unbalanced microbiome not only will the metabolic fate of the tryptophan change more in favor of the “kynurenine pathway” but even amongst the kynurenine pathway we see a shift from production of kynurenic acid compounds with pronounced neuroprotective properties to quinolinic acid a neurotoxic metabolite.
There seems to be a correlation with certain gut related illnesses which have their basis in an unbalanced microbiome. IBS being one. There’s a strong correlation between mood disorders and the gut biome.
We see that inflammation and unbalanced biome lead to majorly increased quinolinic acid levels. Quinolinic acid seems correlated with diseases like Alzheimer’s and Huntington’s showing a likely neurodegenerative quality.
Now here’s a few more articles that link regular folks to this quinolinic acid theory of mood disorders and mental dysfunction.
This one shows people with suicidal depression have increased microglial quinolinic acid.
 jneuroinflammation.biomedcentral.com
jneuroinflammation.biomedcentral.com
Another linking depression with a unbalanced kynurenic acid/quinolinic acid ratio.
 www.ncbi.nlm.nih.gov
www.ncbi.nlm.nih.gov
This article showing the link between kynurenic acid/quinolinic acid and major depression and schizophrenia.
Now this last article is of interest and there’s more to corroborate this claim. It seems kynurenic acid seems to be a possible contributor to schizophrenia but positive for depression, quinolinic acid is bad for depression and cognitive function.
This makes sense as kynurenic acid is a potent antagonist of NMDA, and from anecdotal reports of people with schizophrenia using ketamine they don’t mix well.
But… People with major depression, quinolinic acid being an agonist at NMDA this explains why Ketamine is working wonders for this population.
Hopefully I’ve articulated that well. At the end of the day we could treat the symptoms of the problem as is done with ketamine or we can go right to the source. In this case balancing ones microbiome could mean the difference between depression and possible cognitive problems later in life, or not…
In my next post I’d like to discuss more on how one actually goes about that.
-GC
“The ‘gut-brain axis’ represents a complex network of pathways interconnecting the gut and the brain, comprising the central nervous system (CNS), the sympathetic and parasympathetic branches of the autonomic nervous system (ANS), the enteric nervous system (ENS), as well as the wide array of cells in the gastrointestinal microenvironment.”
“An exciting emerging issue is that the extension of this microbial influence to the CNS may contribute to the regulation of brain development and behaviour.”
“Tryptophan is an aromatic amino acid containing an indolic group attached to an alanyl side chain. The aminoacid is essential for animals and humans, which prevalently derive it from exogenous sources, such as dietary nutrient intake, and, only in part, from endogenous protein degradation. The main dietary sources of tryptophan are chocolate, cereals milk, milk derivates, red meat, poultry, eggs, fish, and dried fruits.”
“In the gut, the amino acid may be also metabolized, under direct or indirect control by the microbiota, giving origin to several compounds, such as 5-HT, kynurenines, tryptamine, and indolic compounds, which participate in the microbiota-gut-brain communication.”
“Under normal conditions, about 90% of the assumed tryptophan is catabolized and transformed into kynurenine through the kynurenine pathway, while approximately 3% is metabolized into 5-HT, and the remaining is degraded by the gut microbiota to produce indole and its derivatives.”
“…metabolites of the kynurenine pathway, collectively called kynurenines, in particular quinolinic acid and kynurenic acid, may influence neuronal activity both in the CNS and in the periphery, retaining neurotoxic and neuroprotective properties, respectively. In this perspective, an unbalanced kynurenine metabolism has been suggested to underlay development of microbiota-gut-brain axis disorders.”
“Quinolinic acid may act as an excitotoxin both in the peripheral and CNS, due to its agonist properties at ionotropic glutamatergic N-methyl-d-aspartate (NMDA) receptors. Quinolinic acid increases extracellular glutamate levels and acts synergistically with the amino acid to induce NMDA-mediated excitotoxicity.”
“A growing body of evidence suggests that quinolinic acid may participate in the pathophysiology of several psychiatric and neurodegenerative disorders. In contrast, kynurenic acid is considered to be neuroprotective, acting as an antagonist at NMDA receptors both in the CNS and in the ENS.”
“Both in IBS and IBD, changes in the microbial community and in its metabolites participate in dysfunctions of the epithelial, immune, and neuronal gut compartments. It is now assessed that such derangements may not only underlay gut symptoms but may also influence the gut-brain communication, predisposing to CNS disorders. In this scenario, impaired tryptophan metabolism along the microbiota-gut-brain axis may potentially participate in the manifestation of both local and CNS symptoms associated with both diseases.”
“IBS patients may frequently experience high levels of anxiety and depression with respect to healthy subjects, regardless of the IBS subtype. Both psychiatric disorders are closely related to stress, an important pathogenic factor for IBS.”
“From a metabolomic stand point, changes in microbiota composition during chronic stress is associated with the diversion of tryptophan metabolism from the 5-HT to the kynurenine pathway. Administration of the probiotic Lactobacillus reuteri in mice subjected to stress stimuli attenuated the unbalanced tryptophan transformation, reinforcing the concept that the microbiota may influence metabolism and resilience during stress.”
“Interestingly, anxiety-like behaviours developed in mice receiving gut microbiota from depressed patients in parallel with increased blood kynurenine levels and kynurenine/tryptophan ratio.”
“Manifestation of depressive symptoms in IBS patients was correlated with altered tryptophan metabolism.”
“Kynurenine involvement in stress-related disorders may depend on the ability of this molecular pathway to influence NMDA receptors located in CNS regions involved in the development of depression, such as hippocampus, amygdala, and cingulate cortex.”
“In mice, the prodrug, 4-chloro-kynurenic acid, induced a rapid onset of antidepressant effects, displaying a better safety profile than other glutamatergic antagonists already used in clinical settings, such as ketamine, holding promises for use in humans.”
“In the gut, the modulation of the kynurenine pathway in favour of kynurenic acid synthesis may be neuroprotective to compensate for inflammation-induced increased NMDA receptor activity in the neuromuscular compartment.”
“Quinolinic, as a neurotoxic NMDA agonist, has been suggested to participate to depression development. Data from clinical investigations suggest that kynurenic acid/quinolinic acid ratio may represent an index of neuroprotection, and a reduced ratio may be indicative of inflammation-induced depressive disorders.”
Tryptophan Metabolites Along the Microbiota-Gut-Brain Axis: An Interkingdom Communication System Influencing the Gut in Health and Disease
The ‘microbiota-gut-brain axis’ plays a fundamental role in maintaining host homeostasis, and different immune, hormonal, and neuronal signals participate to this interkingdom communication system between eukaryota and prokaryota. The ...
“Quinolinic acid…is often implicated in the pathogenesis of a variety of human neurological diseases. QUIN is an agonist of N-methyl-D-aspartate (NMDA) receptor, and it has a high in vivo potency as an excitotoxin.”
“Free radical generation and oxidative stress are involved in the QUIN-induced toxicity; however, we need to take in mind that these mechanisms can be dependent and/or independent of its activity on NMDA receptors. In this line, it has been shown that QUIN can produce oxidative damage independent of its activity under NMDA receptor; this mechanism involves a complex between QUIN and Fe2+.”
“Inflammatory events are also implicated in the QUIN toxicity. It is known that microglia is responsible for inflammatory responses in the CNS and takes the major role in altered levels of QUIN…”
“…large amounts of QUIN are produced and secreted by activated microglia. During CNS inflammation, QUIN levels increase in brain homogenate (246-fold) and extracellular fluid (66-fold).”
“Several reports have been shown that the intrastriatal administration of QUIN in rats produced significant behavioral changes.”
“On the other hand, the few studies in which it has been investigated the cognitive deficits of rats with QUIN lesions have indicated that this metabolite causes deficits in spatial reference memory.”
“Alteration in QUIN levels has been implicated in different pathologies such as Alzheimer's, Huntington's, and Parkinson's diseases..”
Quinolinic Acid: An Endogenous Neurotoxin with Multiple Targets
Quinolinic acid (QUIN), a neuroactive metabolite of the kynurenine pathway, is normally presented in nanomolar concentrations in human brain and cerebrospinal fluid (CSF) and is often implicated in the pathogenesis of a variety of human neurological diseases. ...
GC- Alright that’s enough quotes for a minute. In a nutshell what are these two articles saying?..
The serotonin that our bodies need to function at homeostasis is derived from tryptophan which is more or less produce by microbes in our gut.
With an unbalanced microbiome not only will the metabolic fate of the tryptophan change more in favor of the “kynurenine pathway” but even amongst the kynurenine pathway we see a shift from production of kynurenic acid compounds with pronounced neuroprotective properties to quinolinic acid a neurotoxic metabolite.
There seems to be a correlation with certain gut related illnesses which have their basis in an unbalanced microbiome. IBS being one. There’s a strong correlation between mood disorders and the gut biome.
We see that inflammation and unbalanced biome lead to majorly increased quinolinic acid levels. Quinolinic acid seems correlated with diseases like Alzheimer’s and Huntington’s showing a likely neurodegenerative quality.
Now here’s a few more articles that link regular folks to this quinolinic acid theory of mood disorders and mental dysfunction.
This one shows people with suicidal depression have increased microglial quinolinic acid.
Severe depression is associated with increased microglial quinolinic acid in subregions of the anterior cingulate gyrus: Evidence for an immune-modulated glutamatergic neurotransmission? - Journal of Neuroinflammation
Background Immune dysfunction, including monocytosis and increased blood levels of interleukin-1, interleukin-6 and tumour necrosis factor α has been observed during acute episodes of major depression. These peripheral immune processes may be accompanied by microglial activation in subregions of...
Another linking depression with a unbalanced kynurenic acid/quinolinic acid ratio.
Reduction of kynurenic acid to quinolinic acid ratio in both the depressed and remitted phases of major depressive disorder
Low-grade inflammation is characteristic of a subgroup of currently depressed patients with major depressive disorder (dMDD). It may lead to the activation of the kynurenine-metabolic pathway and the increased synthesis of potentially neurotoxic metabolites ...
This article showing the link between kynurenic acid/quinolinic acid and major depression and schizophrenia.
Now this last article is of interest and there’s more to corroborate this claim. It seems kynurenic acid seems to be a possible contributor to schizophrenia but positive for depression, quinolinic acid is bad for depression and cognitive function.
This makes sense as kynurenic acid is a potent antagonist of NMDA, and from anecdotal reports of people with schizophrenia using ketamine they don’t mix well.
But… People with major depression, quinolinic acid being an agonist at NMDA this explains why Ketamine is working wonders for this population.
Hopefully I’ve articulated that well. At the end of the day we could treat the symptoms of the problem as is done with ketamine or we can go right to the source. In this case balancing ones microbiome could mean the difference between depression and possible cognitive problems later in life, or not…
In my next post I’d like to discuss more on how one actually goes about that.
-GC

