mr peabody
Bluelight Crew
- Joined
- Aug 31, 2016
- Messages
- 5,714

Samoon Ahmad M.D.
Magic mushrooms and the future of psychology
by Samoon Ahmad M.D. | Psychology Today | 22 Jul 2020
A conversation with Stephen Ross about the frontiers of psychological research.
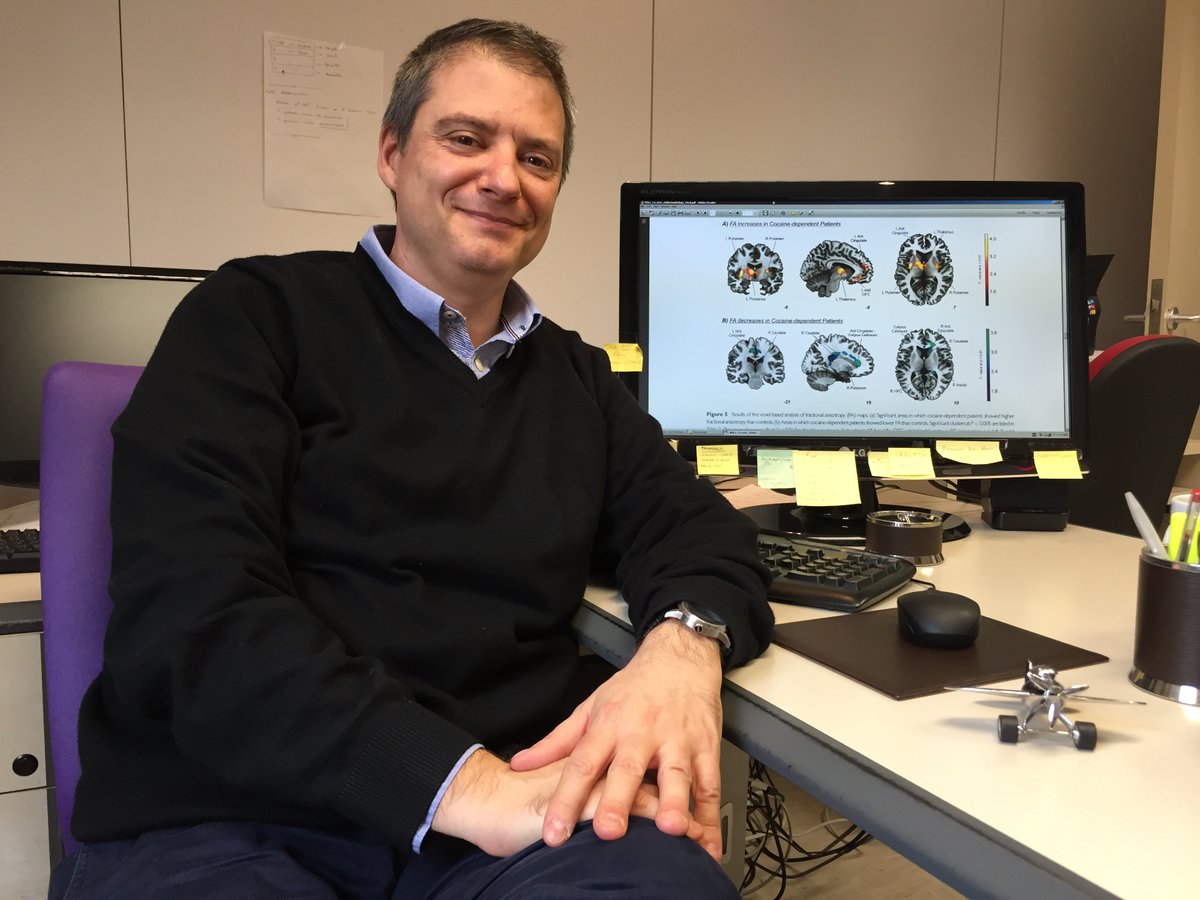
The following is an abridged version of Dr. Ahmad’s recent interview with Stephen Ross, M.D. Dr. Ross is the Director of Addictive Disorders and Experimental Therapeutics Research Laboratory at NYU and an Associate Professor in the Department of Psychiatry at the NYU Grossman School of Medicine.
Dr. Ross has conducted extensive research into the effects of psychedelics, for example psilocybin on addiction and cancer-related existential distress.
Dr. Samoon Ahmad: To start, could you give me a little bit of an overview about what drew you to psilocybin?
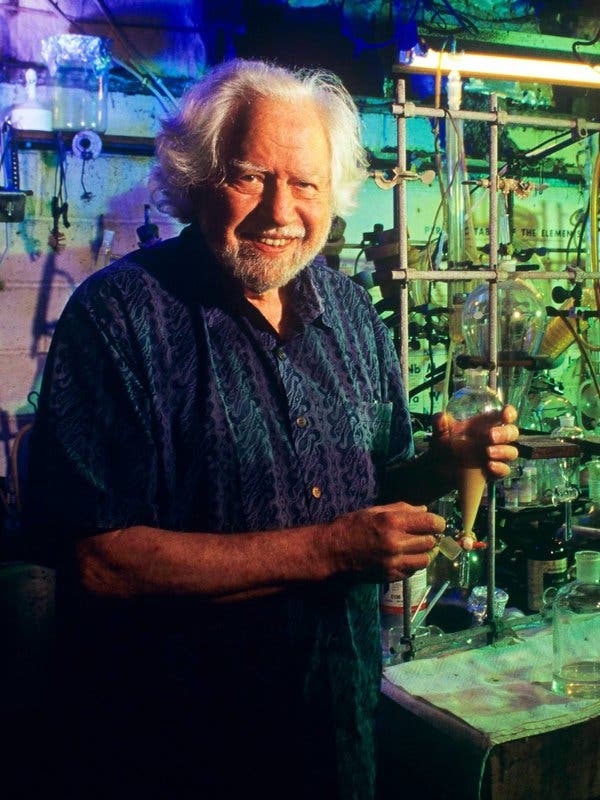
Dr. Stephen Ross: I had just taken over the leadership of the Substance Abuse Division and I was being supervised by Jeff Guss, who’s a longtime faculty member. One day in supervision he starts talking to me about some conference he’s going to in Switzerland commemorating the discovery of LSD. I was like, "What are you talking about? Why would anybody commemorate the discovery of LSD?" And he said, "Well, actually, psychedelics were a big part of psychiatry."
So, I started looking, and you don't have to look very far because it's all kind of hidden in plain sight. There’s this enormous body of research in psychiatry spanning 30 years. There were APA conferences dedicated to LSD; it was hailed to be a wonder drug, and it was used in all these clinical indications. What really got my attention was that the most studied indication with LSD was the treatment of alcoholism.
There were thousands of people in clinical trials. What they found was that a single dose of LSD led to improvements in drinking compared to placebo even after six months. I just thought that was fascinating. The other most studied indication for LSD was for the treatment of terminal cancer—specifically psychiatric and existential distress.
I just thought all this was so fascinating that we decided to form a reading group. We called ourselves the Psychedelic Reading Group at NYU. About a month after we formed the group, I heard that psychedelic research had resumed in the US in the late 90s and that one of the sites was UCLA. Now, I had gone to UCLA for medical school, and my favorite rotation was at Harbor-UCLA, which is kind of like Bellevue. And though I never met him at the time, there was a guy, Charlie Grob, doing psilocybin research for terminal cancer—studying people who had anxiety, depression, and existential distress—at UCLA.
I was introduced to him when I went to visit my family in late 2006. I went to Harbor and we had like a three-hour lunch. He was Division Chief like me, running their child division, and he's just this amazing guy who said, ‘This is a really promising part of psychiatry and it's starting to come back and I'm doing this trial.’ And then he said, ‘Why don't you do a bigger trial at NYU? My daughter is an NYU student. I love NYU.’
You know how much I love Bellevue, but they would not let me do it. I thought that was the end of it, but the NYU College of Dentistry reached out to me, and they said they were interested in part because the head of their clinical research center was dying of lung cancer. So we did this study, this psilocybin and cancer study at the Bluestone Center for Clinical Research at the Dental School.
At the end of that trial, we designed this psilocybin for alcoholism trial, but the dental school said, "We can't have drunk people running around the dental school. You have to do that at Bellevue." And I said, "But Bellevue doesn't allow us to do that." Turns out after several years and positive media portrayals, Bellevue has accepted me back, and so we now have our psychedelic lab at Bellevue. We have several full-time studies. We're finishing up psilocybin for alcoholism. That's going into a Phase 3. We're just starting psilocybin and for major depression. That's a Phase 2. I'm hoping to restart the psilocybin and cancer work soon. We're finishing up use of psilocybin and religious professionals.
Interestingly, in the age of COVID-19, we’re hoping to move in that direction, as well. I designed a trial using psilocybin to treat frontline healthcare workers—you know, ICU docs, ER docs, nurses, and so on—who have COVID-related anxiety, depression, and existential distress. Depending on getting funding, we may be doing something COVID-related.
Dr. Ahmad: In your opinion, are these the kinds of conditions that psilocybin has the most potential to treat?
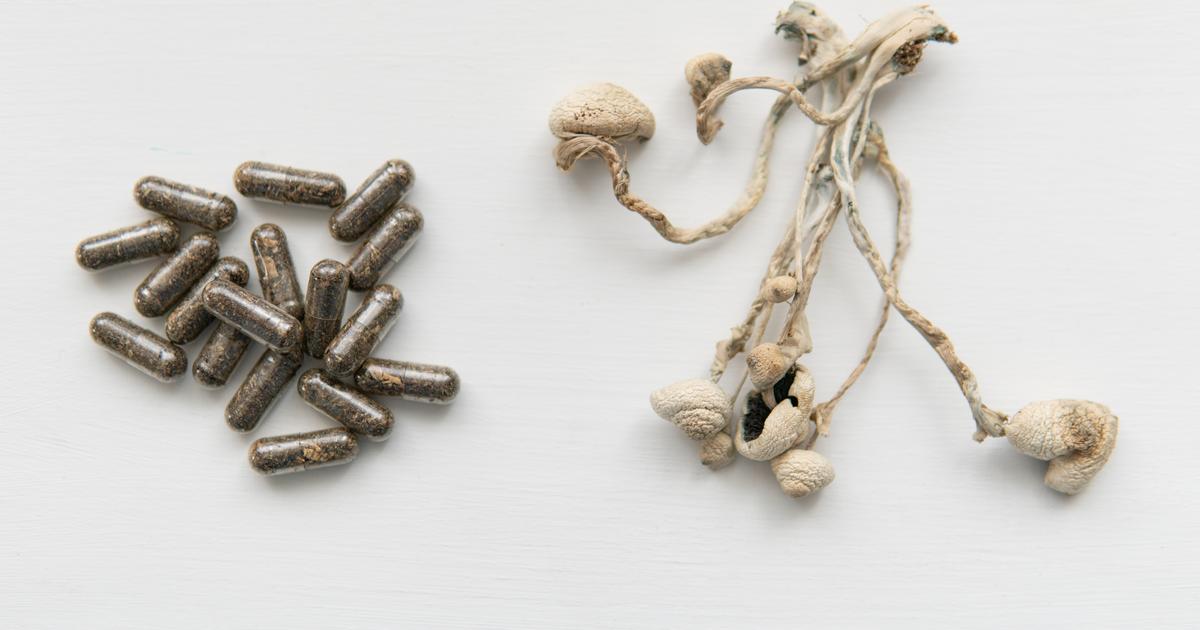
Dr. Ross: Well, there are three main areas that are likely going to get psilocybin rescheduled in the next three to five years: Cancer-related existential distress, alcoholism, major depression. I mean, the trials could fail, but I would doubt it at this point—certainly for cancer and alcohol. We know that there’s a very strong efficacy signal.
We're finishing up the trial on psilocybin and alcoholism in about 100 people, and we’ll analyze the data in a month or so. My sense is that it’s going to be a positive trial. It's going to be helpful compared to placebo. Psilocybin is [also] being studied for tobacco addiction at Johns Hopkins, and they're finishing up a controlled trial of psilocybin versus nicotine replacement, and we'll know more there soon, too. Their pilot trial, you know, was like in 12 people, and it’s astonishing. Like 80 percent of people after two doses of psilocybin were not smoking at six months—but, again, that was open label. It was very small. We have to see what the control trial shows.
There’s also a trial at the University of Alabama finishing up with the use of psilocybin to treat crack cocaine addiction. We should know in a year or so about that. There's now a trial starting up using psilocybin to treat opiate addiction, but that's in the very early stages.
I think psychedelics can be very helpful for addiction. Certainly, that was the most promising area historically, but we'll have to see the results of all these trials to see how helpful they are for these other disorders. If they are, then they’ll have a huge public health impact.
Dr. Ahmad: I’m sort of thinking of the path of marijuana and how long that took to become accepted. Do you think a similar amount of cultural or societal change needs to happen in terms of educating people about psychedelics like psilocybin?
Dr. Ross: I think it's going to be vital to educate the public. Otherwise, history will repeat itself. When psychedelics escaped from the lab and started to be used by the general public, people realized that these drugs were dangerous. Because of that, they were demonized and thoroughly repressed.
Now they're coming back and it’s like the echoes of history. There's this exuberance phase and the public is hearing about it through the Pollan book and other sources, and they're thinking, “My God! This is going to cure me. One or two doses of psilocybin will cure me." And then they realize it's not legal, so then they find it in the underground.
And now you get into dangerous territory. I think if we're not careful, we can have a cultural backlash again. I think what we need to do is be very cautious. Continue to do the research, to do good research to see what the data shows and how good or not the effects are, and then educate the public that, yeah, these are new treatments, but they have risks associated with them and they should only be used in these kinds of ways.
I think the right model is that this is medication-assisted psychotherapy. All our treatments are done with two dyad therapy teams, and there is an enormous amount of preparation before the dosing session.
On the dosing day, you know, it's very controlled. There's a kind of living room in the Clinical Translational Science Institute. We make sure they're ready. We then give them the pill. We turn on preselected music that we play for the whole time. We have them lying supine on the couch. They put eye shades on, they listen to the music, and the default is to focus internally while the two therapists are there to support them.
With psilocybin, it’s a six-hour experience. It comes on gradually, it peaks for about two or three hours, and it comes down gradually. Following the dosing session with the psilocybin, there's a lot of integrative psychotherapy. I really think that the arc is at the heart of the therapeutic experience. The drug is part of it, but the drug facilitates the psychotherapy as opposed to the model of ketamine for depression, which is that it's a biological effect that is changing glutamate or BDNF [brain-derived neurotrophic factor].
Our cancer patients—and this is throughout the study—75 percent said the experience was the single or top-five most meaningful most spiritual experience of their lives. I think these are highly memorable, difficult, transformative experiences that kind of get people thinking in a different way, and then it's what happens after that's key. So, again, I think it’s drugs plus psychotherapy and not just drugs alone.
Months, sometimes years, later we ask them to reflect on the experience, and they're often able to say, precisely, "I had this experience. I remember this thing happening and that's stuck with me to this day. It had a profound effect on me at the time and it still has a profound effect on me. I can remember very clearly when I had that confrontation with cancer" or "When I experienced my death" or "When I came to another insight." And that's why these are so memorable. They have this kind of spiritual content to them.
Dr. Ahmad: You recently published your long-term follow-up study on the treatment of existential distress in patients with life-threatening cancer. Could you share some of your key findings?
Dr. Ross: Yes. The original sample was about 30 and we were able to follow up with about half of them, about 15 or 16, because the other half had died. It was pretty astonishing. Four and a half years after a single dose, we found pretty much what we found one day after giving them the dose. It was that 80 percent of people were in remission from their depression or anxiety symptoms.
But... you have to be very skeptical of that. To really demonstrate that you need a much bigger study. It needs to be a parallel design. But the idea that people with cancer who have a very bad reaction with it, who feel anxious and depressed and wish they were dead already or that life has no meaning, it appears that psilocybin really works for those people. In the majority of them, it can rapidly transform them out of that state and into a much better orientation to cancer and life, and that it can last for a long time.
Dr. Ahmad: Have you found that these spiritual experiences are any more or less pronounced in people who are not struggling with the issue of personal mortality?
Dr. Ross: Well Hopkins did a study they published in 2006. They gave psilocybin to normal volunteers. They didn't have any psychiatric problems, but these were spiritually oriented people. In that study, they found that three out of four said the psilocybin experience was the singular or among the top-five most spiritual or most meaningful experiences of their lives.
Our religious professional trial that we're doing with Hopkins, these are, again, “normal” volunteers, but they’re rabbis, priests, imams. We're still analyzing the data, but, just anecdotally, they've been some of the most profound experiences I've seen. These religious professionals are having really intense spiritual and mystical experiences and they are having, for the most part, a positive impact on their religious practice, and sort of deepening their religion or giving them new insights into the nature of reality and God. So I think that the use in “normal” volunteers is interesting to consider and how it may help people that don't necessarily have a psychiatric illness, but want to have some kind of spiritual growth.
Dr. Ahmad: For patients who have a negative experience, what do you do to manage them?
Dr. Ross: We have a whole algorithm to deal with somebody having a difficult psychological experience. Interestingly, psilocybin is extremely safe medically. It's not associated with organ damage or overdose death. It can cause a mild increase in blood pressure and we measure that a lot, but the main thing is that people can have anxiety reactions or psychotic-like experiences. That's why we carefully rule out people with psychotic illnesses or a family history of these illnesses. We rule out people with severe personality disorders. We also rule out people where there is not a good rapport.
We're very careful to only go into a dosing session if we feel comfortable. If somebody does have a difficult experience, we’ve rehearsed it ahead of time. 'If you feel like you're going crazy and you're never going to come back, that's common. If that happens, this is what you should do: Dive into the experience, don't run away from it. Try to go with it and be curious as the first step.' If they're still having a hard time, we will then sit them up and we might provide therapeutic touch to them. Somebody may hold their hand or their shoulder and reassure them that they’re under the influence of a drug and that they are going to be okay.
And those are often the therapeutic moments. If someone is having a really hard time and they're resisting, and we remind them, 'Go back into it. Don't be scared. We’ve got you.' It's typically those moments that people have these kinds of psychological breakthroughs.
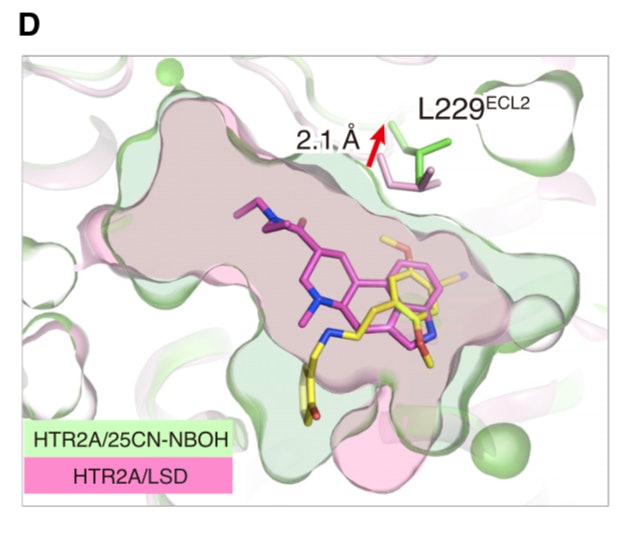
If someone is really having a hard time though, we can give them Valium, but we rarely have to do that—maybe two or three times in 150 patients. If we need to abort the experience, there is an anti-psychotic you can give them. Psilocybin is a 5-HT2A agonist, and we have Zyprexa, which is a 5-HT2A antagonist. If we give them that, it will essentially stop the experience. I think we've done that once.
Dr. Ahmad: Are there any directions that you hope the research will take in the future?
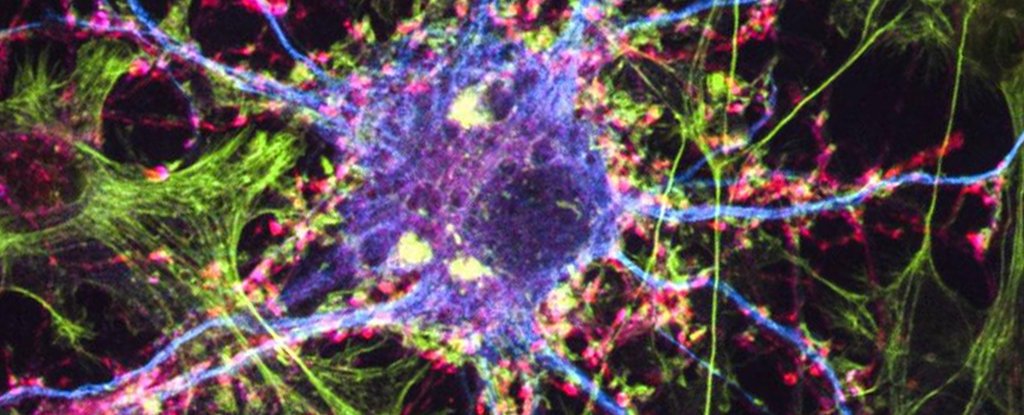
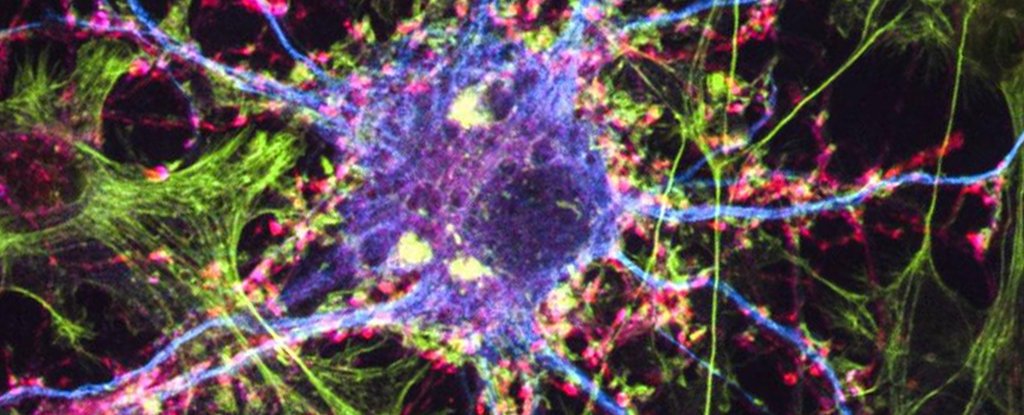
Dr. Ross: We're getting close to forming a Center for Psychedelic Medicine at NYU, and the novel direction we want to go is to use psychedelic therapeutics within medicine and neurology—or at the intersection between psychiatry and medicine. This is an area that is completely new, and this would be for pain disorders. There's evidence that psychedelics have potent anti-inflammatory properties, so we're going to be looking at inflammatory conditions like rheumatoid arthritis and some of these kinds of conditions, too. There's also some evidence that psilocybin is associated with neural regeneration, and there are some people now thinking of using it for neurodegenerative disorders like Alzheimer's or Parkinson's.
The anti-inflammation stuff is interesting. It comes from studies of a psychedelic drug called DOI down at LSU by guy named Chuck Nichols. He took rats that had asthma. When you biopsy them before they get the drug, there’s all this inflammation and all these inflammatory cells. When they gave them DOI, one dose of it, a day later they did the biopsies again of the pulmonary tissue, and what they found was remarkable: There was no more inflammation. All the inflammatory cells were gone. The entire inflammatory process was not there.
Psychedelics exert their psychological effects by activating the serotonin 2A receptor, but how they work as anti-inflammatories is actively being worked on. It definitely appears that they have rapid and sustained anti-inflammatory properties, but there's a lot more research to be done there to see if that's true effect, how universal it is, and then what the exact mechanism is.
It’s wild to think of utilizing them not for their psychological effects, but for their biological effects. And I think the area that, to me, encapsulates putting all this together would be this use of LSD in metastatic cancer pain. There, LSD may have direct analgesic effects, but it also may indirectly help pain by making depression and anxiety better.
So, yeah, the interface with medicine and neurology, I think, is the newest thing. There’s also this concept of microdosing. Rather than these big macro-doses that cause mystical experiences, how can you leverage things and use them daily? There's a lot of hype about LSD and psilocybin microdosing, but there's no data. Those trials are starting.
I was invited by the Journal of Psychopharmacology because they did a review article on microdosing. I think my title was like ‘All Hype, No Data, and the Implications of Microdosing Within Psychiatry.’ It's funny. My mom, who’s in her seventies, asked me, ‘Do you think I should microdose with LSD?’ And I was like, ‘Mom! What are you talking about?’ And she goes, ‘I hear it's great. It's been proven to be great!’
So it just goes to show you that there’s so much out there, and that people think that it's going to help their creativity and their energy and their sex lives and their sleep and on and on. The reality is we know nothing about microdosing. We don't know anything about its potential benefits or its potential harms. If you give a psychedelic a lot, it may be harmful. The serotonin 2B receptor that psilocybin also activates is associated with valvulopathy [disease or disorder of the valves of the heart]. That’s associated with, like, the Fen-phen drug; that was a [serotonin] 2B agonist.[ii] So it may that we find out that microdosing causes cardiac problems, but we just don't know.
People are now just beginning to look at microdosing in human populations, number one, to take normal volunteers and see what are the psychological effects; and then, right around the corner from that group, there are those starting to design trials for microdosing to see if it can help treat psychiatric disorders like major depression, ADHD, addiction.
With microdosing, we just don't know. It's one of these examples of the over-exuberance among the public. People think that something is a real thing, they want to try it, and then they get into trouble.
I have another research program with CBD (cannabidiol), and we're using that daily to treat pain disorders. There's psychedelics, like bromo-LSD as an example, that don't cause any psychological effects, but appear to be helpful for cluster headaches.
Dr. Ahmad: Could psychedelics be used to reduce levels of anxiety and stress?
Dr. Ross: I think so. There's the whole inflammatory hypothesis of depression—that depression is associated with hyper-activation of cytokines and increased inflammation. People with depression have shorter rates of survival compared to people without depression.
We looked at this in cancer. We actually looked at inflammatory and immune markers because cancer-related distress, whether anxiety or depression, is associated with decreased rates of survival, so the implication is that there's something going on We know that depression, in particular, drives this hyper-inflammatory response and decreases immuno-response, but unfortunately we never got to analyze those samples because of Hurricane Sandy. When Sandy hit Bellevue, our samples were in the Bellevue CTSI (Clinical & Transitional Science Institute) and because all the generators are in the basement, and, as you remember, the lights went out, so we lost our samples. We never we never got to analyze them. It would be really interesting to…and, again, this is, like, you have to be very careful here because there really is no data yet, but some people get really excited that psilocybin will cure cancer—not just cancer anxiety, but that it'll make their anxiety and depression so much better that their immune system will get better and they'll fight off the cancer.
That's a real stretch, but you could look at that. You could properly design a trial to actually look at that, and if that were the case, it would be pretty big. But I would think that just improving someone’s state of mind that has cancer is going to have some positive effect on the rate of survival.
Dr. Ahmad: I want to thank you for enlightening us. I really appreciate it. I also want to thank you again for the very kind words about my marijuana book, which is now scheduled to come out September 9.
The full interview was published on Dr. Ahmad’s site, samoonmd.com. You can read it here.

Magic Mushrooms and the Future of Psychology
A conversation with Stephen Ross about the frontiers of psychological research.
Last edited: