Technology Networks
Psychedelic drugs have long been exiled to the fringes of medicine, dismissed as recreational drugs with limited therapeutic potential. That all changed with the breakthrough therapy status granted last year to psilocybin, the active compound found in psychedelic mushrooms, for its ability to rapidly reverse treatment-resistant depression. This has led to an explosion of interest in the field, with new institutes opening and new disorders identified as targets for psychedelic therapy. In our latest interview series, we discuss the potential of psychedelics to revolutionize clinical neuroscience with thought leaders in the field.
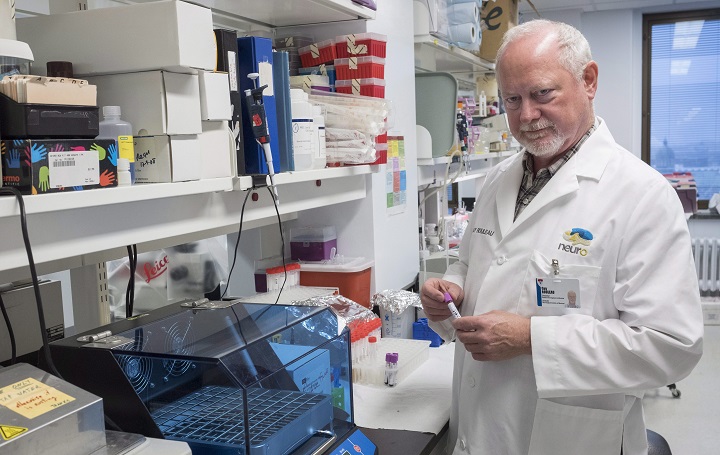
Professor David Nutt, Edmond J. Safra Professor of Neuropsychopharmacology at Imperial College London, has never been afraid to stick his head above the parapet on the topic of drugs. His repeated calling-out of the failures of contemporary drug policy has seen him butt heads with
academics and
politicians alike . But there are signs that opinions about the use of drugs in science and society are tilting at last. The opening of Imperial’s Center for Psychedelic Research, where Nutt is Deputy Head, was one clear indication that the wider field is becoming more open to the therapeutic potential of psychedelics. In this interview with Professor Nutt, we discuss pot, policy and the potential of psilocybin.
Ruairi Mackenzie (RM): Two major new centers for psychedelic research, at Imperial and Johns Hopkins, have been established in the last year. How significant are these developments for psychedelic research?
David Nutt (DN): I think it’s great that there are centers being set up in academic institutions, that’s why we set ours up. The main thing about them is the fact that they’ve been set up in two of the top medical research institutes in the world essentially says that psychedelic research is now accepted as a major branch of medicine, particularly in psychiatry and neuroscience. That’s why they’re so important.
RM: Another recreational drug that has become more widespread in research is cannabis, but the science of cannabis seems less established than the recreational cannabis industry, which has taken off in the US. Do you think the that acceptance of a drug in clinical and recreational use are linked inextricably or are they separate issues?
DN: Well I think the point to make – I think this is a fundamental point, the most important thing I’m going to tell you – is that our research on the neuroscience of psychedelics was the reason we then moved into the clinic, because our first studies on psilocybin, using FMRI imaging, showed surprising, unexpected brain effects which were predictive, we thought, of it being antidepressant. This antidepressant trial, funded by the MRC, that we conducted was predicated on the neuroscience. It was translational science. The brain changed in the same way as it changes with frequency of depression, so we tried it in depression. It’s forward translational science. That’s completely different from cannabis, where that drug has been widely used therapeutically and eventually the medical profession was dragged screaming and protesting to use it. I believe that our science of psychedelics, particularly psilocybin, has been the driver for us doing it, but it’s also given other people the confidence to move it to the clinic because it is no longer just based on self-report from anecdotes of people using mushrooms in their living room.
RM: The studies involved in using psychedelics are very different from casual use and generally their safety seems to require a controlled environment in which they can be taken therapeutically. Is there a way to make these drugs safe to take outside that environment?
DN: One of the reasons we were allowed to do the psilocybin depression study was that I persuaded the MHRA that psilocybin was a very safe drug, because we know about a million young people in Britain a year use mushrooms and there’s very little harm.
I have no worries about people using it recreationally, but I do have worries about depressed people using it recreationally because we have found that the effects of psilocybin in depression are usually very difficult, painful and challenging and I would not have been comfortable with people self-medicating in the middle of a mountain in Wales with mushrooms if they go through the kind of trips that our depressed patients went through. If you’re using these for medicine, you need to have appropriate psychotherapy and medical cover. If you’re using them for recreation, well as long as you’re aware of the risks and you’re not suffering from major mental illness, they’re probably relatively safe.
RM: With the treatment of mental health disorders, it seems unlikely we’ll find some kind of cure-all. Which indications are psychedelics most promising for?
DN: Pretty much all the trials have been done with psilocybin and the areas of clear efficacy are depression – that’s our trial – smoking cessation – that was the Matt Johnson [a Professor at Johns Hopkins] trial and alcoholism, that’s the Michael Bogenschutz [of NYU] trial.
There are also two rather beautiful studies that were blinded studies done in anxiety and depression in people who are facing end of life stress, done by Johns Hopkins and by New York University. Those are the best indications we have at present. There’s also been one rather nice ayahuasca study. Ayahuasca is a preparation of [the psychedelic] DMT. It’s usually used in Latin America, so with ayahuasca, there’s been a Brazilian study showing that Ayahuasca can work in depression.
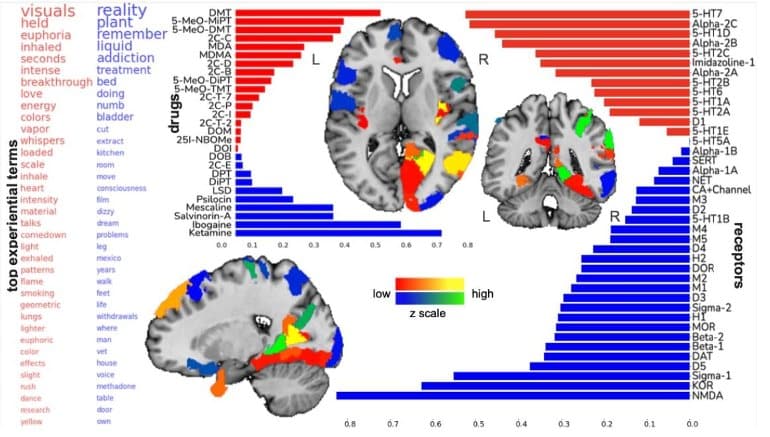
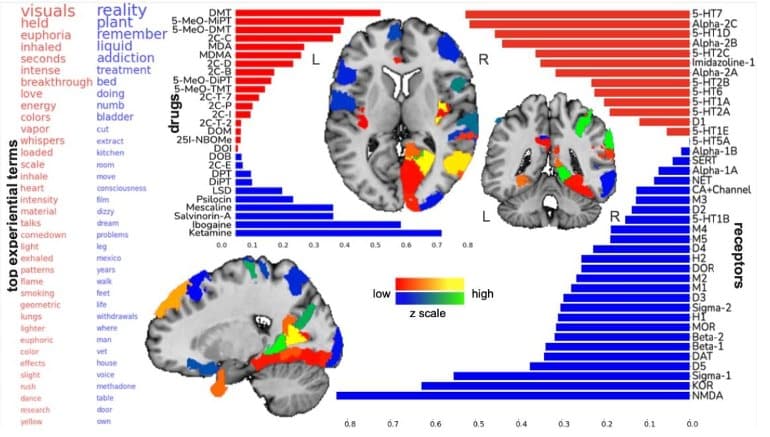
What links depression, tobacco, smoking and alcoholism, we believed - this is our theory – that in these three indications people’s brain gets locked into a way of thinking from which it is hard to disengage. Smoker’s crave cigarettes; they think about cigarettes enormously when they’re trying to stop, or when they have stopped. Alcoholics crave alcohol; their brain is consumed thinking about alcohol and depressed people’s brains are consumed by depressive ruminations. The common factor in those three disorders is the inability of the brain to disengage from maladaptive brain processes.
What psychedelics do in the actual trip itself is have a powerful disrupting effect on brain circuits which underpin those repetitive processes. It’s that disruption that allows people to escape from disorder. Our belief is that any disorder that is accompanied by what you might called locked-in overthinking, could respond. That could also include other forms of addiction, like heroin addiction. We’re teeing up to do a heroin study soon, but also OCD, where people are over engaged in avoidance and fear of responding, avoiding the fearful consequences.
I do not believe psychedelics will be helpful in disorders such as ADHD or schizophrenia or bipolar disorder, but they will be I think useful with disorders that are internalizing disorders. Disorders where people get locked into an internal mindset from which they can’t escape. We’re also setting up to do a trial in anorexia where people have an excessive preoccupation with body image.
RM: Are there any myths around these drugs that you’d like to disperse?
DN: Yes! The first is the continual lying about the fact that these are addictive. The United Nations say they’re addictive, the FDA say they’re addictive, the Misuse of Drugs Act says they’re harmful and addictive. These drugs are anti-addictive. They do not cause addiction. One of the reasons they are banned is because people said they were addictive when they’re not; they
treat addiction. They don’t
cause addiction. The reason they don’t cause addiction is partly because they treat addiction and partly because they produce a very rapid tolerance or desensitization and that occurs so fast that people stop using. There’s a very nice study the US military did, where on the third day the effects wore off. It is one of the reasons they don’t use it in warfare because they realized the Russians could pre-treat their people to develop tolerance for a couple of days. They don’t cause dependence; they don’t cause addiction.
The other myth is they make you crazy. They don’t make you crazy. They might make people who have a propensity to be psychotic more psychotic, but they don’t produce enduring changes in people, negative changes in people’s mental state. If anything they tend to produce enduring positive changes in people. The third myth of course is that they’re very dangerous but as far as I can see there’s almost no deaths from these drugs ever in the history of the world, except from misadventure and of course it is definitely not wise to be taking a psychedelic when you’re sitting on the cliffs in Dover, like a couple of kids did a few years ago at Beachy Head. It’s very silly to go to a place where you are at risk if you’re tripping. In hospital settings, in controlled settings, recreationally these drugs have a low propensity to cause harm.
RM: Psychedelic drugs were very much made out to be dangerous in the 1970s and 1980s, which has hindered research. Is this kind of demonization driven by policy makers or can science play a role now in making sure those same mistakes aren’t repeated?
DN: The demonization was all political, it all goes back to the Vietnam War, to the fact that young men didn’t want to fight in a war in a place they’d never heard and didn’t want to fight against an enemy they’d never seen for a cause they didn’t understand and they refused to fight. They went to San Francisco, they listened to the Grateful Dead, they took acid and they started the anti-war movement. LSD is the only drug that has ever been banned because it changed the way people voted! In those days, you couldn’t ban a drug just because people were using it, you had to find harm. The hysteria about the harms of psychedelics was all created by the drug enforcement agency and the CIA that justified banning it. Once LSD was banned as is almost always the case, they tried to ban every other drug which might be used instead of it. They banned psilocybin, they banned DMT etc. The banning of these drugs is a political act and it was opposed by many scientists at the time.
RM: Will the establishment of large centers like the ones at Imperial and Hopkins stop scientists being ignored again?
DN: It’s a great question. I think you need to ask scientists that, they don’t usually tell me the truth. If they like what I do they say it’s great, but if they don’t, they rarely confront me because I’m quite combative! I don’t know what proportion of scientists are on board with [the centers] but a surprising number of very senior people,professors from top institutions around the world have come up to me, by themselves, shaken my hand and said thanks for doing this, we couldn’t do it, but you can, thank you.
There’s a huge stigma against these drugs. Here’s a true story. I wrote a definitive paper on how the regulations, the scheduling of these drugs destroyed research. I wrote in
Nature Reviews Neuroscience, about five years ago. The journal contracted it and said the condition was I had to get an American author. I rang up a friend of mine who works in this field in America and I said, great news, we’re going to be contracted to write a
Nature Reviews Neuroscience paper on how the drug laws impede research and they said to, “Oh thanks David, but if I put my name to this paper I will never get a grant from the NIH, so I can’t do it. If I do this, they will believe that I’m fighting them, and they won’t fund my research.”
Of course, they’re not funding psychedelic research anyway, but they wouldn’t fund the other research this person was doing. In the end I had to find an American, I found
Dave Nichols, even older than me, who was prepared to. He was past getting grants and he was prepared to write it with me. The pressure from NIDA (National Institute on Drug Abuse) and the NIAAA (National Institute on Alcohol Abuse and Alcoholism) and the NIMH (National Institute on Mental Health) on scientists in America to comply with the status quo, which is that these are dangerous illegal drugs, is stopping research.
RM: A final question on another big story – the licensing of esketamine to treat depression – what is your take on these findings?
DN: It’s very exciting. The thing you need to know about esketamine is it probably works in the same way initially as psilocybin. It disrupts repetitive thinking in depression. It produces similar disorganization of brain connectivity as you get with psilocybin but the esketamine effect doesn’t last very long. It only lasts two or three days. You have to take it twice a week. The [therapeutic] effects of psilocybin, they last for weeks, months or years, not in everyone but in some people. The reason for that is that 5-HT2A receptor which is the target of psilocybin is the receptor which allows you to think differently. esketamine basically causes a disruption of brain functioning, but it doesn’t activate the recovery process whereas psilocybin does.
RM: Do you think the same designation that’s been given to esketamine will be given to psilocybin based on these more enduring results?
DN: I hope so. There is another fundamental difference. The esketamine is given to people who have not fully responded to an SSRI, but you cannot use psilocybin in those people because SSRIs block the effect of psilocybin. The methodology for the psilocybin trial is that you’ve got to get people off the SSRIs, which is quite difficult sometimes. Esketamine is a sort of top-up, where psilocybin is a different, more powerful medication which you have to have people free of other medication to be able to use it. They will be used in quite different populations, I think.
Professor David Nutt has never been afraid to stick his head above the parapet on the topic of drugs. His repeated calling-out of the failures of contemporary drug policy has seen him butt heads with academics and politicians alike. In this interview with Professor Nutt, we discuss pot, policy...

www.technologynetworks.com