mr peabody
Bluelight Crew
- Joined
- Aug 31, 2016
- Messages
- 5,714

Why the future of mental health care may lie in psychedelics
by Rosie Mattio | Forbes Agency Council | 9 Jun 2020
Despite the fact that most non-COVID medical research and funding has come to a halt during the pandemic, there is one emerging field that is still forging ahead. The legal use of psychedelics to treat severe cases of psychological disorders, including depression, addiction and PTSD, has exploded in popularity among researchers and investors in the past two years and has garnered even more interest in recent months.
In just a handful of years, the perception of psychedelics’ brand image among mainstream audiences has rapidly shifted from a dubious party drug to an approachable form of medicine.
Cannabis executives across the industry, including myself, have been monitoring these advancements in hopes that Schedule I substances like cannabis and psychedelics can one day be accepted by mainstream communities as essential forms of medicine.
Psychedelics secures the support of the FDA and medical community
Unlike medical cannabis, which is still navigating a litany of federal research restrictions, psychedelic substances, including ketamine, psilocybin and ibogaine, have been granted FDA approval for clinical trials. In fact, in 2018 and 2019, the FDA designated psilocybin, the psychoactive compound found in mushrooms, as a “Breakthrough Therapy” to treat clinical depression. This coveted classification allows the developers of the drug to conduct clinical trials with more regulatory support and fast-tracks the development and review of final treatments.
Last year, the FDA also approved a ketamine nasal spray to treat depression. The medication has been embraced by psychiatrists across the U.S. and is a breakthrough in its own right, since patients with severe cases of depression can now reimburse part of their legal ketamine treatment through insurance plans, a policy that is unheard of with medical cannabis.
The rising popularity and approval of ketamine therapy in the medical community has also resulted in a proliferation of ketamine clinics in the past few years. Private companies have started opening their doors in major cities in an effort to destigmatize psychedelic medicine and make treatments more accessible. In response to social distancing guidelines, some companies have recently pivoted to telemedicine services. For example, at Mindbloom, a Manhattan-based private clinic, qualifying patients are mailed sublingual ketamine tablets and monitored by a trained clinician over video conference. Considering how some states do not even permit medical cannabis delivery, these advancements in psychedelic medicine reflect how regulators and society may be more open to modern approaches in mental health care than we previously thought.
Investor intrigue fuels industry funding
Although most industries, including cannabis, are experiencing a considerable decline in investment during this period of economic uncertainty, psychedelics have been relatively impervious to recent investing trends. In March, two psychedelics companies, Champignon Brands and Mind Medicine Inc., went public on Canadian stock exchanges. MindMed, which aims to treat addiction and ADHD through ibogaine and LSD, notably raised $24 million ahead of its IPO this year. Bruce Linton, the former CEO of Canopy Growth, was an early investor, which reinforces the importance of legal cannabis and psychedelics growing in tandem.
At the beginning of May, PayPal co-founder Peter Thiel led a $24 million funding round for ATAI Life Sciences, one of MindMed’s main competitors aiming to make psilocybin more scalable and accessible in clinical settings. Similarly, Compass Pathways, a company that was granted the “breakthrough therapy” designation by the FDA for its psilocybin depression drug, raised $80 million in its Series B in April. Another vote of confidence for the industry came from Canaccord Genuity, an investment bank known for funding promising emerging markets, when the company hosted its inaugural virtual Psychedelic Conference Series at the end of April.
Investors may favor psychedelics over cannabis due to the relative regulatory support the industry has received and higher barrier to entry. Risk-averse investors who watched cannabis companies battle with regulators and struggle to recover their stock prices likely view psychedelics as a more controlled and unsaturated environment. Investors are also considering the long-term returns of the industry, as experts estimate that the market for anxiety and depression treatment will reach $19 billion in the U.S. by 2026. For conservative investors, the psychedelics industry is a lucrative branch of pharmaceutical science that may be perceived as more credible due to consistent backing from the FDA and medical community.
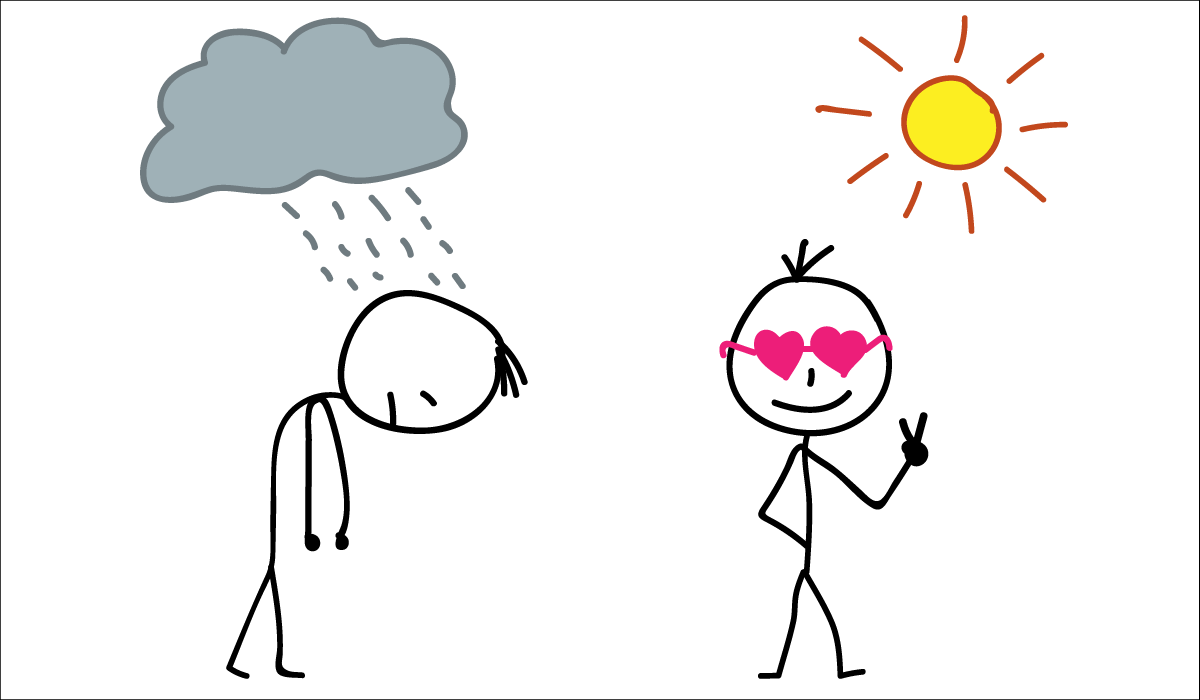
Rising mental health cases will keep psychedelics research in high demand
The National Institutes of Health estimates that over 16 million Americans struggle with depression. Considering the marginal amount of money allocated to mental health care in the national stimulus package, the existing mental health system will be inundated with the number of cases that will certainly increase in the next few months. This, coupled with the fact that nearly 30% of depression cases are treatment-resistant, means the demand for more effective therapies will also escalate in a post-COVID world.
As the world grapples with the aftershocks of the pandemic, patients and healthcare providers will likely seek out alternative and modern mental health services to treat severe psychological disorders. The cannabis industry remains hopeful that their peers in the legal psychedelics space will pave the way for formerly illicit substances to be embraced as innovative medical treatments by regulatory and scientific communities. Individuals struggling with their mental health ultimately deserve to explore every avenue to recovery without social stigmas getting in the way.
Last edited: