The Guardian | 22 May 2022
Clinical trials show that curcumin, present in the spice, may help fight osteoarthritis and other diseases, but there’s a catch – bioavailability, or how to get it into the blood.
While Kamal Patel was probing through the reams of user data on
examine.com – a website that calls itself “the internet’s largest database of nutrition and supplement research” – before a planned revamp later this year, he discovered that the most searched-for supplement on the website was curcumin, a distinctive yellow-orange chemical that is extracted from the rhizomes of turmeric, a tall plant in the ginger family, native to Asia.
Patel concluded that this was probably because of curcumin’s purported anti-inflammatory properties.
“An astounding number of people experience inflammation or have inflammation-related health conditions, and curcumin and fish oil are two of the most researched supplements that can sometimes help,” he says.
This consumer interest in curcumin hasn’t gone unnoticed by the “wellness” industry. Besides its use in pill supplements, curcumin is increasingly being incorporated into cosmetic products that claim to help treat acne and eczema, prevent dry skin, and even slow down the ageing process.
Some reports predict that the global curcumin market size could reach $191m (£156m) by 2028.
The ground rhizomes of the turmeric plant are commonly found in curry powder, but turmeric has also been part of Ayurvedic medicine – a traditional Indian system of treatment – for centuries, and at some point in the last decade turmeric worked its way out of the spice cupboard and took its place at the forefront of the western wellness industry.
“As part of the general concept of Ayurvedic medicine and wellness, it’s increased in popularity in lockstep with yoga and meditation,” says Patel.
Turmeric has become the wellness industry’s new cure-all. It has been subject to all kinds of wild and wonderful health claims, including the ability to relieve allergies, prevent cancer, improve heart health, reverse cognitive decline, cure depression and increase longevity.
As with any dietary supplement, separating the hype and the truth is not straightforward, since not all the claims about turmeric are complete hyperbole. Most are based on the curcumin turmeric contains, which has been shown to be a
potent anti-inflammatory and antioxidant.
This is where it gets more complicated. The proportion of curcumin in turmeric is just 3%, by weight. The scientific studies that have made positive health associations use either pure curcumin or turmeric extract that has been designed to contain mostly curcumin. The doses of curcumin required to give benefit are very high – typically about 1,000mg a day. So despite what manufacturers might claim, consuming turmeric shots and lattes or adding a little extra spice to your meals will not come close to reaching the necessary dose. Some turmeric products have even been found to be
contaminated with heavy metals such as lead, which can have adverse effects on your health.
But there is genuine interest from scientists around the world in curcumin’s potential as a natural treatment for a whole range of chronic illnesses. The most convincing evidence so far relates to its ability to
relieve joint pain in people with osteoarthritis, an area of medicine where there is a huge unmet need owing to the limitations of non-steroidal anti-inflammatory drugs (NSAIDs).
“Osteoarthritis is the most prevalent joint disease worldwide,” says Kristopher Paultre, assistant professor of orthopaedics and family medicine at the University of Miami.
“NSAIDs have been a staple in treatment but are not without their drawbacks including gastrointestinal, cardiac and renal issues when used chronically.”
But this is just one area of investigation. There are 70 clinical trials around the world that are either active or seeking patients, and are looking at the potential of curcumin to treat chronic kidney disease, cognitive decline, irritable bowel syndrome (IBS), macular degeneration, and even to slow down the progression of various forms of cancer.
Turmeric lattes are promoted as a healthy alternative to coffee but the evidence is questionable.
Advances in drug-delivery techniques
In the mid 1990s, Jack Arbiser and Nancy DeMore were young researchers at Harvard Medical School exploring new treatment options for cancer, when they came across some research suggesting that curcumin could inhibit the growth of different types of cancer cells in a test tube.
Intrigued by this, they went on to find that curcumin could
prevent the formation of new blood vessels, a process called angiogenesis, which all tumours require to sustain themselves.
“Together we showed that curcumin inhibits angiogenesis,” says DeMore.
“We were very excited about this initial finding. There have since been several studies using curcumin in clinical trials in patients with pancreatic cancer, breast cancer, and multiple myeloma showing that there is some biologic effect.”
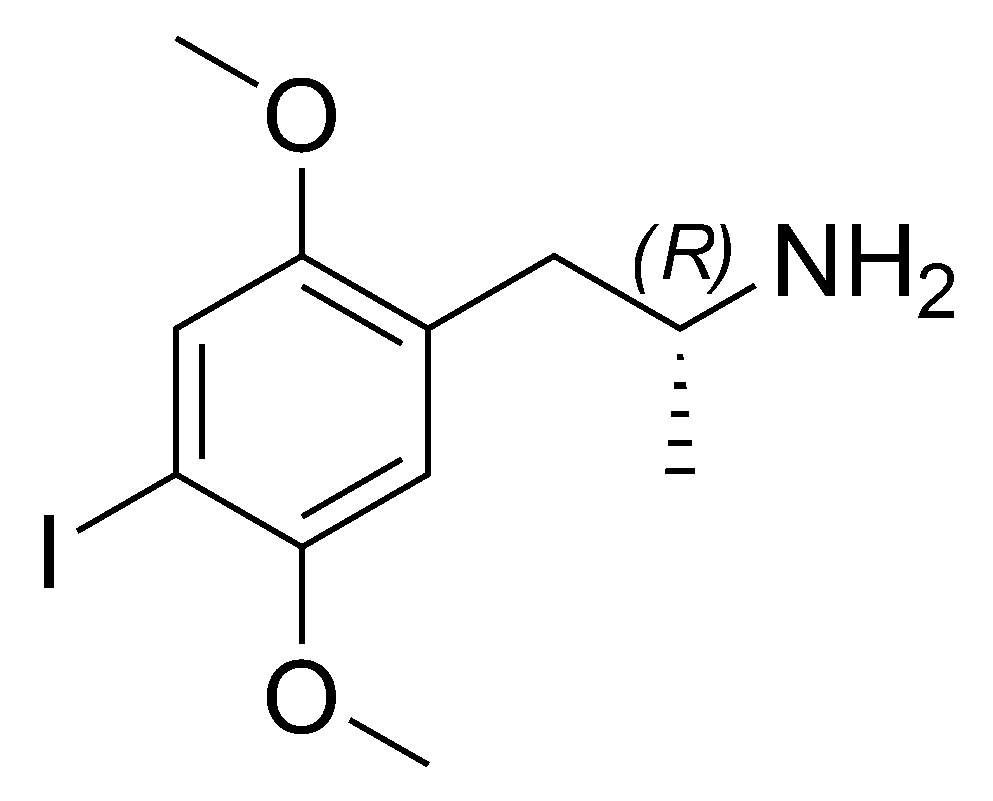
However, when scientists moved from testing curcumin in the lab to testing it on humans, there was a catch – one that has dogged curcumin ever since. The compound has notoriously poor bioavailability – the rate at which the body absorbs a substance – making it nearly impossible to get sufficiently high concentrations of curcumin into the blood through oral supplementation alone. This, along with the commercial difficulties of patenting natural products, meant that scientific interest in curcumin soon waned, and would remain in the doldrums for more than a decade.
But in recent years, advances in drug delivery techniques have renewed interest in curcumin.
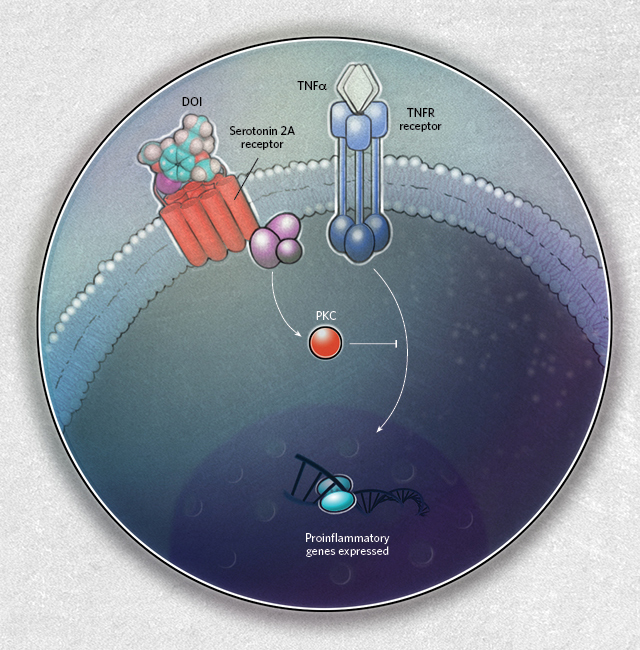
Nanoparticle systems are being explored as ways of potentially getting high doses of curcumin to tumours. Some research has shown that combining curcumin with piperine – a compound found in black pepper –
can enhance its absorption into the blood, although it still remains to be proven whether this can help yield benefit in humans. While there are now a whole variety of off-the-shelf supplements that combine curcumin and piperine, there are still challenges for scientists looking to use it medically. One of these is that piperine
has been shown to inhibit a variety of enzymes that aid in metabolising drugs, and it remains to be seen whether this could cause an increased risk of side-effects in patients also taking prescription medicines.
“The problem of curcumin’s absorption has been enthusiastically addressed by a number of supplement companies and researchers,” says Wyatt Brown, a researcher at examine.com.
“They typically do this by packaging it in highly absorbable lipids of various types so that more of it gets into the body.”
This has been accelerated by a drive for more natural alternatives to painkillers, but also by the fact that in the world of sport, curcumin has gained a reputation as an aid to muscle rehabilitation. Scientists at Northumbria University are planning a clinical trial to study this, while in the US, Paultre is already witnessing the rise of curcumin as a sports supplement.
“Curcumin has seen a significant increase in use in athletics for recovery post-workouts and after games,” he says.
“The idea is the same as with osteoarthritis and the goal is to reduce inflammation. We tend to avoid chronic NSAID use in athletes due to side-effects. The evidence seems to be positive, but once again there is still work to be done.”
Potential new delivery methods have sparked interest once again in curcumin’s potential anti-cancer properties, with various researchers keen to explore its uses in patients in the early stages of the disease, as an add-on treatment to more conventional cancer drugs.
DeMore, now a professor of surgery at the Medical University of South Carolina, has returned to studying curcumin after a near 20-year gap, launching a clinical trial to see whether breast cancer patients taking a formulation of curcumin specially designed to enhance its absorption into the blood experience a decrease in tumour proliferation.
At the same time, oncologists at the University of Rochester Medical Center in New York state are running a trial to see whether curcumin supplemented with piperine can halt disease progression in patients with low-grade prostate cancer, and prevent them from requiring more aggressive treatment.
In both cases, scientists are keen to emphasise that these trials are very much in the exploratory stage, and even if they produce positive results, far more proof will be needed before curcumin can be officially recommended for cancer patients. For example, even if the data from DeMore’s study shows that curcumin appears to reduce the rate at which tumours are growing, it would then require a full randomised control trial – where curcumin is compared against a placebo – to prove that it can actually prolong survival or prevent tumour recurrence in cancer patients who have been through chemotherapy.
“The problem is that many of these natural products have not been through the traditional clinical trials to evaluate whether or not they truly are effective,” says DeMore.
“If our trial shows benefits, it would allow us to write grants to fund further randomised controlled clinical studies.”
Paultre says it is positive that further independent trials are being funded for curcumin because much of the research on the compound has been acquired through small studies that have been financed by the nutraceutical industry, which has created a perception of curcumin as a miracle cure.
“Current studies still have a lot of potential bias in them,” he says. “Nutraceuticals do not have much regulatory oversight, and companies want to make a profit. There is always concern for bias in these studies, which produce amazing results with a specific product.”
While there is ongoing interest in curcumin across a whole spectrum of diseases, there is a lack of concrete evidence for its benefits for conditions such as cognitive decline, IBS, or chronic pain beyond osteoarthritis, while Wyatt describes any claims that curcumin could meaningfully reduce the risk of cardiovascular disease as “speculative”.
But there are hopes that the anti-inflammatory properties of curcumin could offer benefits for depression. Laura Fusar-Poli, a psychiatry researcher at the University of Catania, Italy describes a number of theories, including that curcumin may be able to restore levels of serotonin in the brains of depressed patients and a possible modulatory effect on the brain-gut axis. But to date, evidence of any of this in humans remains scarce.
Paultre is hoping that the current interest in curcumin will help develop a gold-standard way of delivering it into the body as well as agreements on the best dose to use, which could all make it easier for scientists to quantify its benefits in future.
“The problem is that there is no consensus on appropriate curcumin levels for therapeutic effect,” he says.
“Additionally, with so many formulations out there, there are no studies comparing the bioavailability of each one. It’s a bit like the wild west in this regard. Therefore though there is evidence of curcumin being helpful in some conditions, there is still a lot of work to be done.”
*From the article here :
Clinical trials show that curcumin, present in the spice, may help fight osteoarthritis and other diseases, but there’s a catch – bioavailability, or how to get it into the blood

www.theguardian.com