Albert Hofmann
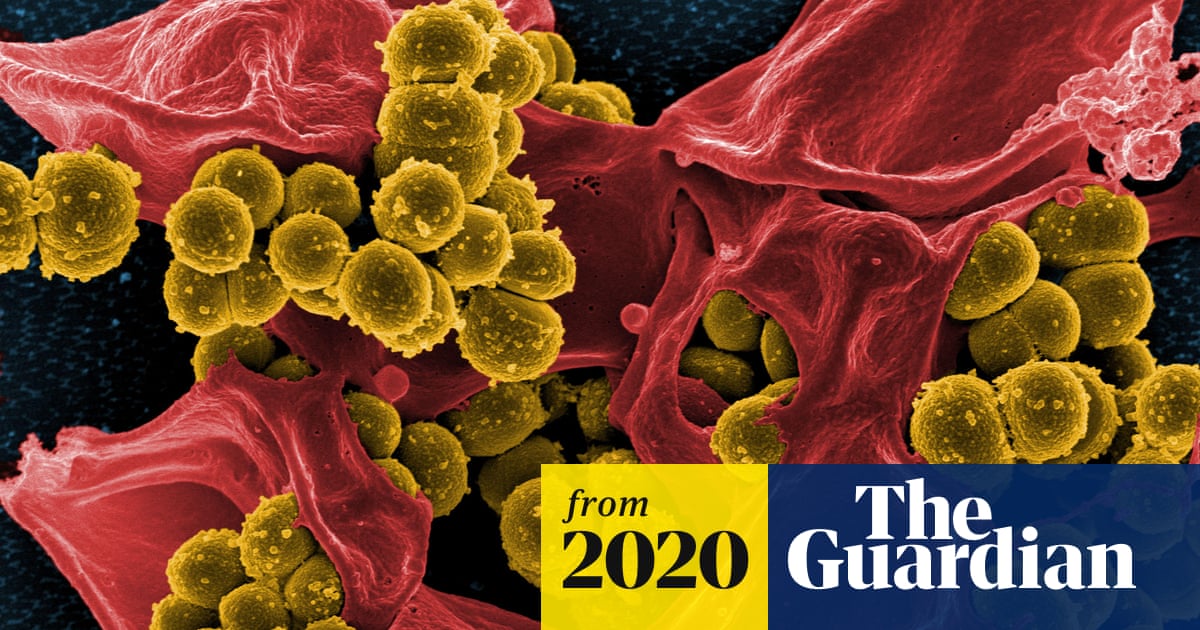
Anti-viral effects of Ibogaine
Dr. Vic Hernandez
Ibogaine in its administered forms has typically been applied to persons seeking a chemical dependence addiction treatment. The target population not only has had to contend with chemical dependence issues but issues concerning other infections, most notably HIV and/or HCV or co-infection. As antidotal and preliminary scientific information is noted concerning Ibogaine treatments, trends suggest potential applications to these pathogens. Medical science has not rigorously pursued investigation into the potential applications of Iboga alkaloids in
in vitro work, animal and human studies.
I am a public health wonk. I have had the luxury of doing what interests me in what I call Public-Health. I get off on effecting and affecting the public's health. My work in HIV has concerned oxidative stress and HIV and its contribution to the understanding of pathogenesis and pathophysiology. I've been involved in developing guidelines for physicians treating HIV, trial design and methodology. I have worked on developing practitioner education forums to support understanding and treatment for isolated populations infected with HIV, notably active users. My unique relationship to communities affected by HIV, activism and passion for my work has brought me to unique understandings and relationships that I have brought to other public health work. I received a congressional citation for this work. Working with Lynn Mofenson at the NIH we moved to look at micro-nutrient intervention in HIV non-progressors to affect HIV progression and delay ARV intervention without compromising patient health by allowing HIV to run unabated. The fruits of this work have been born out in the African studies noted in US papers recently. Working with Lynn, Fauzi at Harvard and others, we established a treatment approach that was frowned upon when we started back in 1993 into accepted and respected reality.
Noted work included the resurrection of Alfa Lipoic Acid as a micronutrient effecting Liver toxicity. It would later be applied to HCV cases. In recent years, needing and wanting a break from HIV, I've worked in the realm of cancer, looking at the role of genetics in identifying trends in non-progressors utilizing non-conventional therapies or no therapeutic interventions. This work has allowed me to look at orthomolecular medicine (effect of micro-nutrients on the biochemistry of the body, pathogen infection, self cells run amuck and wellness and quality of life). Working with colleagues and mentors as Lynn Margulis at U Mass Amherst and Walter Willet at Harvard, I began to understand as Lynn puts it: the symbiosis of medicine, and as Walter puts it, as the effect of the basic building blocks of body systems and their abilities to stay healthy. Why mention this blather? You need to know where I am going with this information, so we can understand where we headed, now and in the future.
HIV. Where we are, and what it means
HIV research and treatment approaches have been checkered and somewhat baffling in approach and far too complex to delve into at this meeting or in this short of time. From a conventional medicine perspective, there are three steps required for HIV to enter cells: Attachment, Binding to a co-receptor, and Fusion of HIV into CD-4 cell. The currently available classes of drugs work to prevent the process of HIV reproducing itself and infecting new cells after HIV enters the CD-4 cell: They are Nucleoside Analogues, Non-nucleoside Analogues and Protease Inhibitors. These drugs have been administered in combination, at varied intervals, and in varying doses to tease out efficacy for the particular viral strain(s) expressed by the patient. Toxicities to body systems and healthy cells require strict and watchful management.
There is a new class of drugs called Entry Inhibitors which block HIV from entering CD-4 cells. They work by blocking the HIVs ability to enter and infect a cell. Essentially there are two steps to
entry of HIV into the CD-4 cell. HIV attaches to the CD-4 cell and then fuses with it. After fusing with the cell, HIV can dump its genetic material into the CD-4 cell, the material it needs to reproduce itself in the CD-4 cell. There are two steps to attachment: attaching to the CD-4 receptor and then to a co-receptor, either CCR5 or CXCR4.
Basically, how
Entry Inhibitors work is first by:
- Attachment
- Co-receptor binding
- Fusion
Currently available HIV drugs other than Fuzeon, prevent HIV from reproducing once HIV in the cell.
HIV Super-infection and HIV Drug Resistance. Let's start with HIV super-infection. Studies over the past two years suggest this is a real problem. Super-infection is when a person who has HIV gets infected with a second viral strain of HIV. Super-infection, based on study, occurs 5 to 13 months after estimated date of initial infection. The super-infection strain can be associated with ARV susceptibility and adherence. In some cases, a person can be infected with a drug resistant strain and then become infected with a super-infection wild-type or visa-versa. Initial co-infection cannot be ruled be ruled out. Molecular investigation determines evidence of super-infection coupled with progression and ARV response. The rate of the super-infection based on study hovers somewhere around 6.5% annually. Harm reduction counseling is recommended by the researchers.
There are some in the medical science community that are trying to link the super-infection to a
patient zero that originated from New York.
Nonsense! This was tried at the beginning of the HIV/AIDS pandemic by saying that HIV started in North America with a Canadian airline steward. It is impossible to narrow down such a claim. By the way, in that case, it was refuted by the testing of IDU blood samples from the early seventies that had been banked at Beth Israel. HIV was found in those cohorts, long before the Canadian air-steward stuff. At a recent conference, Paul Volberding MD from UCSF noted that the super-infection business hinged on one reliable case and that the bally-who was uncalled for. This should not minimize sound and reliable public health interventions such as safer sex practices.
Unfortunately, we are learning about HIV pathophysiology and pathogenesis as we go along instead of developing the understanding first. This may deal a blow to 18-MC, if applied to HIV or not.
As for HIV drug resistance, it was not until ICAAC in October of 2004 did the rates found seem alarmingly worrisome. Soon after, the media has grabbed a hold on this information. Studies are finding an escalation of HIV drug resistance during primary infection period (shortly after infection). And the resistances vary among drug classes. Drug resistant HIV acquired at time of infection can establish itself as the dominant virus population and become archived in the latent cellular reservoir. This may result in sub-optimal response to ARV interventions and promote the accumulation of mutations and jeopardize already limited treatment options. In further study, HIV drug resistance has been found in 1 of 7 treated in the US of a cohort of 317 in 40 US cities. The prominent resistance was found in the non-nukes class of drugs. Ethnic differences were noted. Latinos and Asian patients had a lower prevalence of reduced susceptibility (6 percent, with Caucasians at 27 percent, and Blacks at 23 percent. There were no gender differentiations or comparisons done. These were among male cohorts.
HCV and co-infection
HCV therapeutic interventions are limited in pharmaceutical application (interferon and pegalated interferon [riboviron and interferon]) are limited. There are surfacing reports indicating significant efficacy with TCM. In the co-infected individual, treatment options reduce due to the environment of the liver.
When Howard approached me with this paper, I read it and got excited. I like new ideas and approaches especially if the science is tight and is respectful of change. No one has the ace card and false hope, especially for patients, is highly unethical. Ask David Ho MD at Rockefeller's Aaron Diamond Center regarding the premature delivery of HIV cure based on invitro data. After reading the paper Howard shared, the questions flooded through my head and as we talked, he suggested I say a few words. Reluctantly, I accepted. I have been trying to avoid public gigs (especially those that risk pissing contests). The paper (above) by Silva et al from Brazil entitled:
Anti-HIV-1 Activity of Iboga Alkaloid Congener 18-MC is a significant piece of work. It was an
in vitro (in lab) study using human cells. The Iboga alkaloid 18-MC was introduced to human Peripheral Blood Mononuclear cells (PBMCs) and monocyte-derived macrophages. The result was the significant inhibition of isolates of HIV-1 in a dose dependent manner.
The approach of this anti HIV-1 inhibitory activity study went something like this: An
in vitro study of donor PBMCs cells from healthy donors was executed with monocyte-derived human macrophages isolated from the PBMCs. This was not a formal clinical trial with subjects. Materials and methods seemed valid and reliable. Then HIV-1 primary isolates (3) were used. AZT, a nucleoside analogue was used as a control probably because the mechanism of action of 18-MC is as reverse transcriptase inhibitor and AZT is a nucleoside analogue used to affect reverse transcriptase. PBMCs were exposed to viral suspensions of HIV-1 P-24 antigen. Viral replication was assessed by measuring P-24 antigen. Dose ranges from 12.5 to 50 micromolers significantly effected HIV proliferation. Time durations varied from 3, 10, 14 and 21 days. A variety of doses, durations were done to observe safety, and effect. Compared to the control (AZT) which was rigorous as expected, 18-MC faired very well. It should be noted that the infection assays were performed with primary cells (acutely infected PBMCs and macrophages) to avoid the genotypic and phenotypic changes that might occur during viral changes that might occur during viral passages in tumor cell lines. They also used primary isolates, which are phenotypically closer to the viral population present in HIV-1 infected patients. Additionally, they looked at the naturally occurring COR and its anti HIV-1 effect and found significant results, but the data was not reported. They did report the indole alkaloid congener 18-MC molecule of the natural COR, presenting little to none of the adverse effects associated with the original molecule in this antiviral study reported. These study design considerations contributed to a tight study with valid and reliable outcomes.
Basically, 18-MC inhibits HIV-1 replication in human PBMCs and in monocyte-derived macrophages. This antiviral effect of the alkaloids may be due to their action on different steps of viral replication, such as inhibition of syncytium formation and reducing the activity of HIV-1 enzyme reverse transcriptase. So how this applies to the HIV treatment intervention picture is up for grabs. Certainly, further study needs to be done on the mechanisms by which 18-MC decreases HIV replication
in vitro, in addition to inhibition of HIV reverse transcriptase. It is worth doing for a number of potential reasons:
1. 18-MC has a lower toxicity profile compared to the drugs in the study control class (nucleoside analogues). And I would venture to say in the other three classes that prevent the process of HIV from reproducing itself and perhaps infecting new cells after HIV enters the CD-4 cell.
2. 18-MC provides a potentially safe ARV therapeutic intervention in less virulent strains of HIV and minimizing toxicities.
3. Co-therapeutic intervention can be matched with micro-nutrient regimens which have been shown in study to delay ARV therapeutic intervention for up to 5 years, notably in women and infected infants.
4. 18-MC, based on its mechanism of action against HIV in comparable drug classes, could be applied to HIV infected pregnant women to affect mother to fetus transmission rates. The studies among these populations used AZT, the control for the 18-MC. I believe 18-MC has a less toxic profile than AZT even thought AZT showed significant interruption of mother to fetus HIV transmission.
5. Given the pharmacodynamics of Iboga alkaloids in the brain, the potential for crossing the blood brain barrier is significant.
6. As mentioned earlier in Dr. Onaivis presentation, the potential of Ibogaine to regulate inflammation (genetically) is significant for persons living with HIV/AIDS where inflammatory states are hallmark.
7. I believe it would be cost effective in poorer nations struggling with HIV infection.
There are issues here, too.
1. Since this 18-MC affects HIV-1 at reverse transcriptase, such as other classes of drugs, perhaps there is a chance for drug resistance as found in other drugs in that class or a shorter duration to it?
2. Perhaps it can be used in initial therapy in super-infections or drug-resistant strains until it succumbs to those viral expressions.
3. In combination with other drug classes such as nukes, non-nukes and protease, there is a strong potential for side effects. But given their toxicity to body systems and healthy cell lines that the nukes, non-nukes and protease inhibitors have, pairing them up with this group may not be wise. This is dependent on dose levels and state of the patient.
4. Perhaps it can be paired up with the new
Entry Inhibitors to provide a well-rounded combination to thwart HIV. This I see as the most promising combination.
5. In the case of co-infection, particularly for those with HIV/HCV infection and dicey livers, this may prove to be questionable. I believe the verdict is not in, and further research is needed.
6. Regarding potential psychedelic effects, it should be noted that Sustiva reports similar side effects (like hypnogocic hallucinations) and has been controlled through a variety of provider and patient interventions.
What medical science needs to do
Simple, more study, but the politics of what gets studied and how it gets funded are sad realities. But history has shown us that vigilant activism can effect epistemology, study approach even study design and recruitment. For example, a medical treatment support group comprised of non-active injection drugs users (IDUs) based in the Bronx found the Hypericin study at Bellevue Medical Center in NYC to be of interest. But they found the route of administration (subcutaneous) a bit unwelcoming since it brought up potential triggers to use again. They met with the principal investigator (PI) Fred Valentine MD and persuaded him to add an arm that was orally administered. He agreed and they (the patients) help recruit for the study.
Since the study was done in Brazil and not in the US, the chances for further investigation are probably more promising. Based on this limited work, an Investigational New Drug (IND) designation can be developed, funding lined up, bring it up with Community Review Boards (CRBs), cultivate interested researchers are among the many avenues medical science must go with this. Working with the Institutional Review Boards (IRBs), who wheel a lot of political power to support pursuit of an Iboga-alkaloid as an anti-viral. This is most effective if you have a PI lined up with a clear focus, good science under his/her belt coupled with sufficient funding source(s).
What can patients and advocates do?
I believe there are many things that can be done here, to name a few:
1. Brainstorm with constituencies of patients in effected populations. Dr. Ken Alper and others have mentioned the comradery of the group having been treated with Ibogaine. These people serve as a constituency who can affect the fast tracking of treatments.
2. Develop proactive treatment support groups that can be involved in trial design, methodology, trial recruitment, trial implementation, and adherence. For example, I have started HIV/AIDS treatment support groups called AMEN (Attitude, Medications, Exercise, Nutrition). These groups encourage patients to be their own primary healthcare advocate. They are involved in all aspects of patient treatment intervention(s), advocacy, and often times drug development.
3. Treatment support group can not only promote such objects as patients being their own primary healthcare advocate but also informal researchers. For example, setting up simple databases that encourage the observation of trends of persons taking Ibogaine and the effect on say HCV or HIV. Blood work-up can be a point measure to observe trends.
4. Cultivate active and fruitful relationships between the treatment support group members and their healthcare providers, especially when it comes to understanding the population of active and non-active users, their medical conditions and predispositions, and above all the dynamic of behavior notably addiction.
Remember, some of the most profound discoveries and epistemology in medical science have come from non-medical and/or science trained patients and their advocates.
https://ibogainedossier.com/v_hernandez.html