Chronic sufferers choosing psilocybin for migraines
by Michael Chary | GAIA | 7 Mar 2020
I remember the day I got my first migraine pretty vividly. I was a freshman in high school sitting in math class, when all of a sudden, my vision became blurry. I soon felt shaky, nauseous, incredibly confused, and frightened by what was happening to me. But in the hour or two it took to see a doctor, my symptoms had disappeared.
Eventually, I realized I had experienced my first migraine, and since then I suffer through a few every year. While they're pretty debilitating and can ruin an entire day, I'm lucky I don't suffer from chronic migraines like some do.
In the U.S. it's estimated that roughly 3.2 million Americans live with chronic migraines and of that percentage, some experience 15 to 20 a month. These headaches last four hours or more on average, and often force sufferers to take days off work. This adds up to not only lost hours of their lives, but lost productivity and money. In fact, it's estimated up to $31 billion in productivity is lost annually from headache disabilities in the U.S. alone.
I can tell when a migraine is coming on because of a chain of predictable symptoms. First, I begin to see auras and my vision is blurred, then all symptoms subside like the calm before a storm, and finally the piercing headache, nausea, vomiting, and shakiness.
Hallucinations and bizarre visuals often accompany or signal to migraine sufferers they're about to endure a headache. The most common visual oddities are blurriness and auras, but some experience zigzags, swirling vortices, and Picasso-esque patterns. Physical hallucinations arent unusual either.
During his first migraine, author, Anthony Peake, says,
"I felt that the top of my head was lifting off and moving upwards toward the ceiling. Then I noticed the office seemed to be getting smaller, as if I was looking at it from the wrong end of a telescope."
Only about 15 to 20 percent of migraine sufferers experience migraines with auras. These migraines can be so disorienting and confusing, sometimes rendering sufferers unable to communicate properly, almost like a stroke. But despite the well-documented symptoms and prevalence of these painful experiences, doctors still don't know what causes them exactly.
Headache disorders are ranked 7th in all disabilities globally, though only 36 percent of sufferers are diagnosed. And migraines aren't even the worst type of debilitating headache - that title is reserved for cluster headaches.
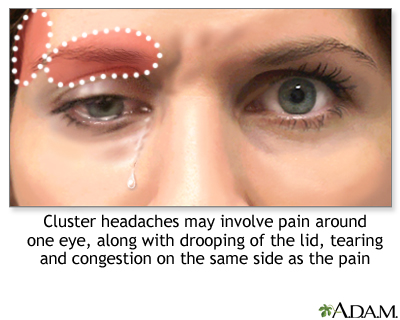
Cluster headaches have been described as one of the worst pains a human being can feel, worse than childbirth, or as one sufferer put it, worse than having a limb amputated without anesthesia. Cluster headaches have been nicknamed the suicide headache for reasons that can probably be inferred.
These two types of headaches tend to occur in one gender more than the other, with migraines choosing women, and cluster headaches more often reserved for men. Some attribute this to hormonal functions, but no one really knows for certain.
Specific things activate migraines, including caffeine, lack of sleep, alcohol, weather fluctuations, and stress. Cluster headaches, on the other hand, seem to fall into episodic cycles, and contrary to migraines, sleeping can actually trigger them. Sufferers often get cluster headaches as they're entering REM sleep, leading them to fear bedtime.
LSD and psilocybin for migraines
Sometime in 2015, well over a decade after my headaches began, I was at a friend's house when I felt the early signs of an oncoming migraine. I alerted my buddies to what would happen and the protocol I typically followed to deal with the next few hours of pain.
My friend Sean said he wanted to make me something that might help my symptoms. So he whipped out his mortar and pestle and began making me a chunky paste, while I laid on the couch, preparing for the impending agony. After a few minutes, he came back with the paste and a glass of water, telling me to consume the strange concoction.
I asked what was in it and he replied,
"Some honey, various herbs, and some (magic) mushrooms. Not enough to make you trip, just a micro-dose, but there's a chance you might feel a body high. It will definitely help your symptoms, though."
Now, full disclosure, I had taken psilocybin before, so I was familiar with its effects, but the idea of a potential psychedelic trip while suffering from a mind-numbing headache sounded like a horrible idea. But I trusted Sean and took the mushroom mixture.
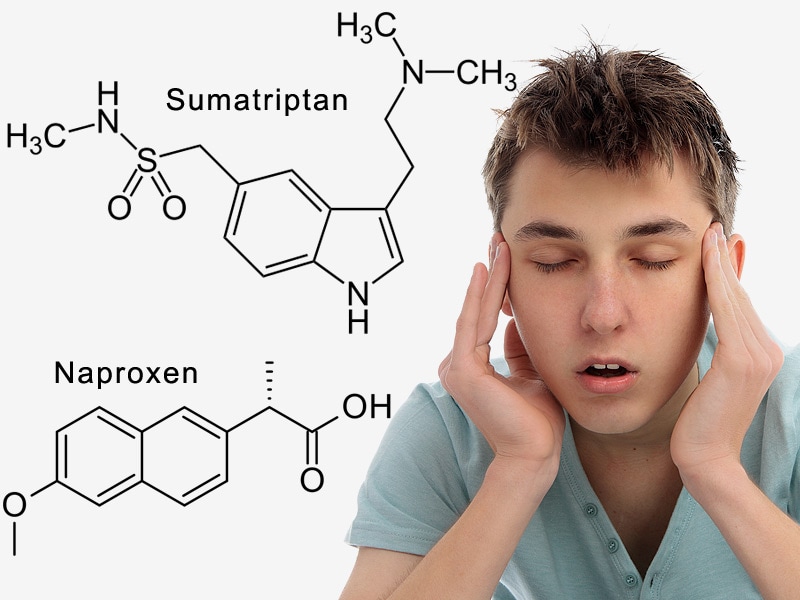
For chronic headache sufferers, there are a number of pharmaceuticals prescribed to mitigate their symptoms and lead a semi-normal life. Triptans are one of the most commonly prescribed, often paired with an NSAID, i.e. aspirin or ibuprofen. But these drugs are not a panacea and only provide temporary relief.
Triptans are referred to as selective serotonin receptor agonists, stimulating serotonin production in the brain. This serotonin increase reduces inflammation and constricts blood vessels to alleviate the headache. Triptans belong to the tryptamine family of monoamine alkaloids. Coincidentally, the psychoactive compounds found in many psychedelics are also tryptamines.
Psilocybin converts to psilocin in the body, becoming a partial agonist for serotonin receptors known as 5-HT receptors, particularly the 5-HT(2b) and 5-HT(2a) receptors. Psilocybin and other tryptamines, including DMT and LSD, are referred to as serotonergic psychedelics because they activate these serotonin receptors. Triptans work as agonists on serotonin receptors in the same way, but instead stimulate 5-HT(1b) and 5-HT(1d) receptors.
For reasons not fully understood, the receptors that psilocybin and LSD target produce a psychedelic experience, while the receptors the triptans target do not. However, when both receptors are targeted, the psychedelic experience can be amplified immensely, but not in a pleasant way.
Unsurprisingly, another pharmaceutical used in the past to treat migraines, due to its affinity for those 5-HT receptors, is ergotamine, a peptide derived from ergot fungus, first isolated by Arthur Stoll at Sandoz Pharmaceuticals in 1918. Stoll worked alongside Albert Hoffman, the famous chemist who first synthesized LSD at Sandoz from, you guessed it, ergotamine.
When Hoffman accidentally synthesized LSD he had also worked to isolate psilocybin from the mushroom Psilocybe mexicana. Sandoz sold psilocybin to clinicians using it for psychotherapy, before the drug was criminalized in 1968. It's believed that Hoffman was actually working on synthesizing new medicines to treat headaches, which he may have apparently found, though the hype from his discovery's psychedelic properties completely overshadowed any other use for it.
After Sean gave me the micro-dose of magic mushrooms, my headache began to play out as expected. My liver had to first process the psilocybin, convert it to psilocin, and release a number of metabolites into my bloodstream; a process that usually takes 30 to 45 minutes. But after that time had passed, it felt like I had skipped the worst part of my headache and was coasting through the dull afterglow that marks the latter stage of my migraines. I also felt a little woozy, the feeling I knew the mushrooms were responsible for.
It seemed Sean's magic mushroom remedy worked. It didn't stop the headache dead in its tracks, but it did mitigate the pain significantly and shorten the span of it. Now, had I been working at the time, the subtle psychoactive effects of the psilocybin may have been distracting, but with a full-blown migraine, no work would have been accomplished anyway.
Cluster Busters - Using psychedelics for headaches
Triptans, steroids, and other pharmaceuticals prescribed to treat chronic bouts can have long-term side effects ranging from organ fibrosis, cardiac disturbances, and even osteoporosis. And while triptans are good for alleviating individual headaches, chronic sufferers have found that psychedelic serotonergics can break or even prevent the episodic cycles of headaches that recur on a predictable basis.
Those unfortunate enough to suffer from cluster headaches experience as many as eight to 10 a day during cycles. Though they don't suffer year-round, cycles typically last anywhere from two to three-months, with each headache lasting anywhere from 45 minutes to three hours.
Bob Wold is the founder and president of Cluster Busters, a group that has, for the past 15 years, advocated for the study and legal use of psilocybin and LSD for treatment of cluster headaches. Wold began suffering from them biannually for a period of 20 years after being misdiagnosed many times. He was ineffectually prescribed 75 different medications, including the highly addictive fentanyl and even cocaine drops.
Wold was so desperate to ease the pain that he almost underwent an invasive, unproven surgery that would have severed his trigeminal nerves and destroyed all sensation in his face. That was, until he found an online forum touting the benefits of serotonergic psychedelics for treating his condition.
Wold said he asked his two kids, who happened to be in college, to procure him the necessary psilocybin-containing mushrooms to see if they could ameliorate his agonizing pain. While he doesn't condone buying psilocybin mushrooms off the street, as acquiring them is illegal and hard to determine exact dosage, Wold was in a desperate state and willing to take risks.
Shortly after using the drug to treat his headaches, Wold noticed an immediate difference, saying his head hadn't felt that good in the 20 years since his condition began. From then on, he used the drug as both an analgesic and a preventative measure, spreading the word to fellow sufferers as often as possible.
Cluster Busters says it believes the key difference between triptans and serotonergic psychedelics is that the receptor targeted by the latter acts as a vasoconstrictor, preventing attacks by keeping the carotid artery from expanding and pressing on the trigeminal nerves.
Unfortunately, taboos and legal constrictions have made it hard to gauge doses and procure these drugs safely for chronic headache sufferers, but recent persistence and overwhelming anecdotal evidence from Cluster Busters has led to legally approved trials of the drugs for treatment of severe chronic headaches.
Researchers like Harvard psychiatrist, Dr. John Halpern, decided to look more closely into the stories being reported from Cluster Busters and conduct a study of his own. After interviewing 53 subjects who used a serotonergic psychedelic to treat cluster headaches, he found that 95 percent successfully delayed or completely avoided headaches. This led Halpern to set up future double-blind studies with control groups to properly test results.
Much like the dose I received from Sean to treat my migraine, the doses used by most cluster headache sufferers are micro-doses, or non-psychedelic doses. Even the slightly larger, preventative doses Wold takes a few times a year , he says, are roughly tantamount to a buzz from a few glasses of wine - enough to make lights look slightly more vivid.
Another strong proponent who deserves mention for use of psychedelics to treat chronic headaches is Graham Hancock. Hancock says at one point he was suffering from up to 20 severe migraines a month, before he took Ayahuasca and Iboga in shamanic ceremonies.
Ayauhasca is an Amazonian brew containing DMT, another serotonergic psychedelic found in many plants. Today, after suffering from chronic headaches his entire life, Hancock no longer suffers from them at all, and has vowed to take Ayahuasca two to three times a year to prevent them, and for the spiritual experience it provides.
Of course, one should tread with caution when considering these drugs for treatment. Wold says it's important to consult a doctor to ensure these psychoactive substances won't react adversely with any other medications one might be on, and to assure that one is healthy enough to take them.
With any luck, further research into serotonergic psychedelics can help relieve the pain for victims of chronic headaches and eliminate the unwarranted stigma placed on a natural substance with medicinal value. For more information visit the Cluster Busters website or MAPS, another group that continues to achieve funding and legal permission to advance clinical trials studying the healing potential of psychotropic drugs.
https://www.gaia.com/lp/content/psyc...for-migraines/