- Joined
- May 11, 2011
- Messages
- 3,378
MDMA interactions with pharmaceuticals and drugs of abuse
I just copied the whole text of this review. It lacks a lot of topics such as 2d6 opioids, psychadelics, and ketamine, but does have into about mdma interaction alcohol, cannabis, caffeine and a bunch of pharmaceuticals.
I just copied the whole text of this review. It lacks a lot of topics such as 2d6 opioids, psychadelics, and ketamine, but does have into about mdma interaction alcohol, cannabis, caffeine and a bunch of pharmaceuticals.
Review
MDMA interactions with pharmaceuticals and drugs of abuse
Esther PapaseitORCID Icon,Clara Pérez-MañáORCID Icon,Marta Torrens,Adriana Farré,Lourdes Poyatos,Olga Hladun, show all
Pages 357-369 | Received 02 Feb 2020, Accepted 26 Mar 2020, Accepted author version posted online: 31 Mar 2020, Published online: 12 Apr 2020
Download citation
CrossMark LogoCrossMark
In this articleClose
ABSTRACT
1. Introduction
2. Data search and selection methods
3. MDMA–drug interactions (MDMA-DIs)
4. Conclusion
5. Expert opinion
Additional information
References
ABSTRACT
Introduction: MDMA (3,4-methylenedioxymethamphetamine), a synthetic ring-substituted amphetamine, has become one of the most widely used recreational psychostimulant drugs in the world. Among recreational ecstasy/MDMA users, polydrug use is a phenomenon whose common purpose is to experience the synergistic effect of the combined drugs, moderate MDMA effects, prevent potential toxicity, enhance a high or come down from a high from other drugs, or simply to treat existing medical conditions. Thus, MDMA–drug interactions (MDMA-DIs) lead to a higher risk of acute and life-threatening MDMA toxicity.
Areas covered: This article provides an overview of the MDMA-DIs with pharmaceuticals and drugs of abuse. In addition, available evidence is summarized along with clinical recommendations. Finally, the increasing importance of MDMA-DIs is highlighted.
Expert opinion: There is a reduced number of published MDMA-DIs studies and scarce clinically significant MDMA-DIs documented in the literature. Experimental evidence points out the relevance of MDMA-DI’s when MDMA is co-administered with pharmaceuticals that are metabolized by the CYP2D6 due to MDMA inhibitory action and in the case of repeated MDMA administration (MDMA-MDMAIs).
KEYWORDS: 3,4-methylenedioxymethamphetamine (MDMA)acute MDMA toxicitydrug interaction (DI)pharmacodynamicspharmacokineticspolydrug use
Previous article
Next article
1. Introduction
It is well known that drug–drug interactions (DDIs) can potentially occur when two or more drugs, including medicines – pharmaceutical products, are taken at the same time by the same subject. Therefore, significant DDIs can result in adverse drug reactions, clinical toxicity, life-threatening episodes, and even fatal consequences. It is important to note, however, that DDIs are not limited to pharmaceuticals; recreational drugs can also potentially interact with pharmaceutics and other recreational drugs taken simultaneously [1]. Whilst DDI assessment, benefit-risk assessment of therapies, and prescribing information are integral parts of the drug development process for pharmaceuticals, for recreational drugs, there are not international recommendations to assess DDIs, neither are there strategies to avoid them. Therefore, concomitant use of either recreational drugs with pharmaceuticals or drugs of abuse is an under-examined source of DDIs. Despite concerns from potential DDIs, recreational drugs are usually used in combination (simultaneously or sequentially) with other/s legal or illegal drug/s (at least two substances) in the same time period, which is broadly defined as polydrug use [2,3].
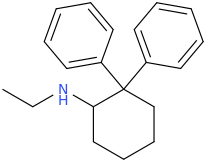
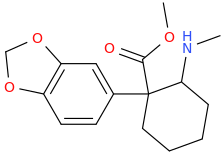
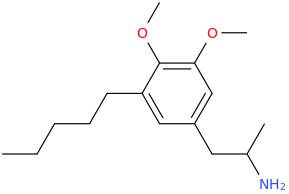
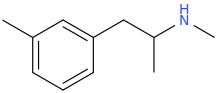
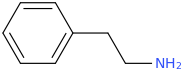
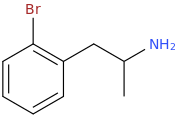
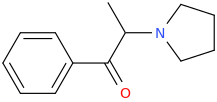
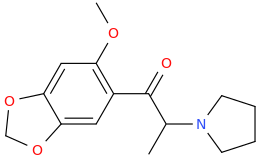
3,4-methylenedioxymethamphetamine (MDMA), referred to as ecstasy, Adam, XTC, or Molly, is a synthetic ring-substituted amphetamine derivative that is structurally related to methamphetamine and mescaline. Despite its current illegal status (listed in Schedule I of the United Nations 1971 Convention on Psychotropic Substances) [4] and the emergence of novel psychoactive substances (NPS), ecstasy has become one of the most widely used recreational psychostimulant drugs in the world. Since the late 1980s, its use has extended among young people mainly associated with recreational nightlife settings, including mainstream clubs, parties, raves, and electronic music dance festivals. More recent estimations of the United Nations and European Drug Report show evidence that MDMA consumption is a worldwide phenomenon with estimated lifetime and last year's use of MDMA/ecstasy varying among adult and young adult population and regional areas. As an example, in North America, it is estimated that 0.9% of the population aged 15–64 were past-year ecstasy users in 2017 [5]. In Europe, roughly 0.5% of the population aged 15–64 is estimated to have used ecstasy over the past year in 2017, with national estimates ranging from 0.2% in Portugal and Romania to 7.1% in the Netherlands, while prevalence estimates for those aged 15–24 years are higher, with 2.3% (1.3 million people) [6].
It is notable to remember that MDMA was synthesized by Merck laboratories in 1912 and in the early 1970's it was discovered its use to enhance the effects of psychotherapy. Lately, the classification of MDMA as a controlled substance made its use in therapy illegal and created serious obstacles to clinical research including assessment of safety. Nonetheless, last year's new research has emerged demonstrating the potential efficacy of MDMA for Posttraumatic Stress disorder (PTSD), as an enhancer of psychotherapy when used under physician control at relatively low doses in comparison to recreational doses [7].
MDMA acts as an indirect serotonin or 5-hydroxytryptamine (5-HT) agonist, inducing serotonin release from neuronal endings and inhibiting its reuptake. In addition, MDMA is a releaser of norepinephrine (NE) and, to a lesser extent, of dopamine (DA) [8–11]. MDMA effects at low doses are primarily considered to depend on its serotonergic effects acting mainly as an indirect agonist of serotonin receptor subtypes mainly through 5-hydroxytryptamine (5-HT) 5-HT1A, 5-HT1B, 5-HT2A receptors and at (slightly) higher doses it robustly affects NE and DA system [12]. Importantly, the latter actions (not mediated by serotonin action), are mostly responsible for the MDMA adverse effects.
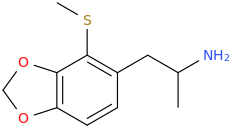
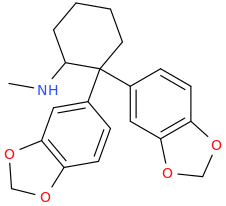
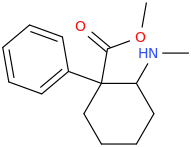
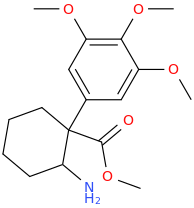
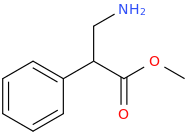
MDMA is predominantly taken orally as tablets or crystal, although it can also be snorted (insufflated) as a powder or injected intravenously. Following oral administration, MDMA is well and rapidly absorbed, and it is mainly metabolized by the liver. It includes primarily two complex metabolic pathways: O-demethylation by cytochrome P450 2D6 (CYP2D6) and other cytochrome P450 isoenzymes (CYP1A2, CYP3A4, and CYP2B6) to 3,4-dihydroxymethamphetamine (HHMA), and N-dealkylation to 3,4-methylenedioxyamphetamine (MDA). MDA is an MDMA minor metabolite (8–9% of the concentrations of MDMA) which is also O-demethylated to 3,4-dihydroxyamphetamine (HHA) [13–15]**. Both HHMA and HHA are either O-methylated in a reaction involving the catechol-O-methyltransferase (COMT) or they form sulfate and glucuronide conjugates. Both HHMA and HHA can partially undergo further autoxidation to the corresponding ortho-quinones, which are conjugated with glutathione to form glutathionyl adducts [14]. The pharmacogenetics of MDMA have yielded some biological insights in relation to mutations in the main CYP isoenzymes involving MDMA metabolism. In relation to CYP2D6, MDMA poses a mechanism-based inhibition that exhibited a reduction of approximately 40% of CYP2D6 activity through the formation of a complex between CYP2D6 and MDMA [16–18] (see section MDMA-DIs with drugs of abuse and social drugs). The disposition of MDMA and its effects in humans are altered by polymorphic CYP2D6 activity, as well as moderate increases in the plasma exposure to MDMA and its active metabolite MDA, and a more rapid onset of associated blood pressure and psychotropic effects in individuals with poor CYP2D6 function. Nevertheless, the effects are small because of the autoinhibition of CYP2D6 [19]. The mutation of the CYP2C19 or CYP2B6 gene that reduces enzyme function has been shown to increase the ratio of MDMA/MDA but it does not alter HMMA concentrations, neither does it modify the subjective response to MDMA. Subjects with decreased CYP2C19 function showed greater cardiovascular responses with faster onset times. This factor could play a key role in the clinical toxicity of MDMA, whereas polymorphism in CYP1A2 does not seem to alter the response to MDMA [19,20]. Genetic polymorphism in genes that encode key targets in the 5-HT system and norepinephrine transporter did not significantly influence the effects of MDMA in healthy subjects [21]. Norepinephrine transporter gene variations did not have a major role in the cardiostimulant effects of MDMA [22]. Oxytocin gene variations may modulate aspects of the prosocial subjective effects of MDMA in humans [23].
When MDMA is administered to healthy recreational drug users under laboratory conditions in placebo-controlled studies, single oral doses of MDMA produce mainly sympathomimetic, stimulant-like and entactogen/empathogen effects. The typical cardiovascular and autonomic effects are characterized by significant increases in blood pressure (BP), heart rate (HR), temperature (T), mydriasis, and esophoria [24–29]. MDMA induces feelings of well-being, euphoria, stimulation, energy, happiness and self-esteem, extroversion, enhanced empathy and closeness to others, increased desire to socialize (prosocial effect), and perceptual disturbances, but not hallucinations [30–34]. Pharmacokinetic data show maximal plasma concentrations (Cmax) values peaked around 2 h (Tmax), and the elimination half-life (T1/2) is about 8–9 h with an apparent calculated volume of distribution (Vd) of 450 L [35].
Real-world clinical features on acute MDMA toxicity include nausea, vomiting, mydriasis, xerostomia (dry mouth), sweating, restlessness, tremor, hyperreflexia, irritability, pallor, bruxism, trismus and/or palpitations [36–38]. According to the literature, moderate ecstasy intoxication is characterized by muscle tension, tachycardia, hypertension, slight increase in body temperature, hyperactivity, confusion, anxiety, and, less frequently, panic attacks and psychosis [29,39,40]. Most severe ecstasy effects are related to cardiovascular toxicity, including rhythm disturbances (atrial and ventricular tachydysrhythmia), hypotension, infarction and sudden death, hyperpyrexia (hyperthermia, hyponatremia), hepatic (fulminant hepatitis), renal (renal failure associated with rhabdomyolysis) and neurological toxicity (coma, seizures, intracranial hemorrhage, subarachnoid hemorrhage, cerebral infarction, and cerebral venous sinus thrombosis), and psychiatric disturbances (delirium) [41–50]. Furthermore, the reported severe systemic toxicity caused by MDMA includes the serotonin syndrome (increased muscle rigidity, hyperreflexia, and hyperpyrexia), heatstroke/hyperpyrexia/hyperthermia (rhabdomyolysis, myoglobinuria, disseminated intravascular coagulation and renal failure) and the syndrome of inappropriate antidiuretic hormone secretion (SIADH) [51–64].
Polydrug use in recreational ecstasy/MDMA users is a common phenomenon described in the context of experiencing the synergistic effect of the combined drugs, moderating MDMA effects (easing the come down from a high), preventing potential MDMA toxicity, enhancing a high or coming down from a high from other drugs, or simply treating existing medical conditions or enhancing performance and image. Traditionally, ecstasy users have frequently reported concomitant use with tobacco and alcohol, as well as cannabis, methamphetamine, cocaine, GHB, and ketamine [65].
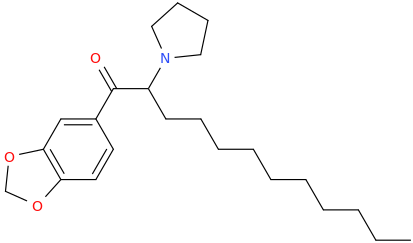
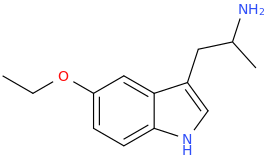
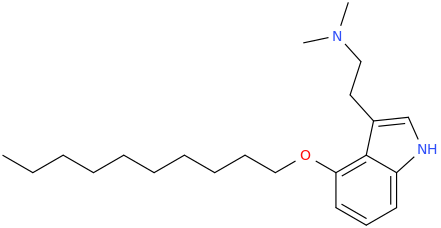
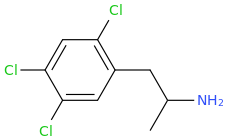
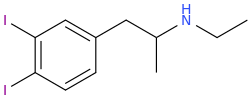
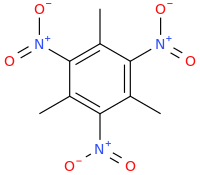
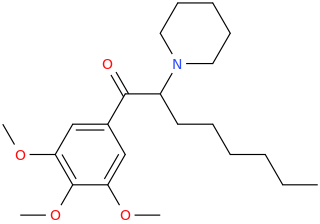
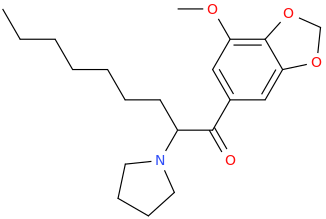
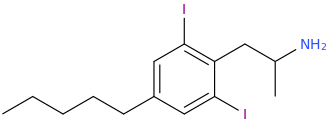
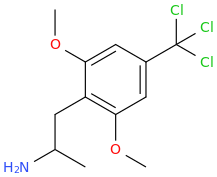
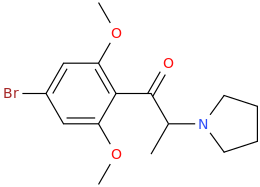
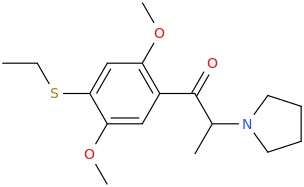
Recently, epidemiological data have revealed different factors added to classical risk factors of acute MDMA toxicity (e.g. high room temperatures >30°C, vigorous activity, and limited access to water or other beverages, MDMA purity, MDMA contamination) that may precipitate or contribute to developing potential MDMA-DIs (MDMA drug interactions) that could result in increased harm and even deaths linked to the use of ecstasy (Table 1): i) an important increase in the MDMA content of ecstasy tablets (up to 200 mg/tablet, usually 50–100 mg/tablet) [66]; ii) the adulteration of ecstasy tablets with other psychostimulant-like substances [(3,4-methylenedioxyamphetamine (MDA), 3,4-methylene-dioxyethylamphetamine (MDEA) and N-methyl-a-(1,3-benzodixol-5-yl)-2-butamine (MBDB), methamphetamine (MA), amphetamine (A), ketamine, caffeine)] [67,68], and certain NPS [meta-chlorophenylpiperazine (mCPP), paramethoxymethamphetamine PMMA)] [5]; iii) the new pattern of binge use of MDMA [repeated MDMA consumption (MDMA–MDMA interactions (MDMA-MDMAIs)] by taking several tablets simultaneously (stacking), or at intervals over a period of time such as an evening or even several days (boosting); iv) and new phenomena such as chemsex [the simultaneous use of MDMA in combination with gamma-hydroxybutyric acid (GHB), inhaled nitrites (poppers), among others] among groups of homosexual or bisexual men and men who have sex with men, and ‘sextasy,’ [MDMA used simultaneously with sildenafil (Viagra®)].
Table 1. Potential sources of MDMA–drug interactions (MDMA-DIs).
CSVDisplay Table
Information about acute health harms related to ecstasy polydrug use comes from epidemiological data, reports from emergency departments (EDs) or from toxicological analysis. Different nightlife and electronic dance music studies have estimated that a non-depreciable percentage of ecstasy users have experienced an ecstasy-related adverse effect or ED attendances associated with concomitant use of other drugs, primarily a combination of MDMA and alcohol (up to 25%) [69–72]. In addition, multiple cases of severe toxicity have been described as life-threatening or fatal MDMA-DIs after suspected or analytical confirmation of the use of MDMA in combination with selective serotonin reuptake inhibitors (SSRI) [73], monoamine oxidase inhibitors (IMAOs) [57,74,75], and antiretroviral agents [76–79].
Despite the wide recreational ecstasy use, the rates of morbidity, disability, and mortality associated with it are relatively low. Evidence shows that the vast majority of potential health harm is linked to polydrug use and, consequently, caused by potential MDMA-DIs. Defining the way in which MDMA acts and mainly interacts with other pharmaceuticals and drugs of abuse may represent an important improvement for understanding its acute toxic mechanisms and clinical implications [80–82]. Over the last decades, MDMA human pharmacology has been investigated in clinical studies assessing its pharmacological profile. Although experimental data on MDMA-DIs with pharmaceuticals and/or drugs of abuse are limited, it continues to be an interesting topic of discussion. The purpose of this review is to examine data on pharmacological MDMA-DIs and their potential importance to guide clinical decision-making in cases of acute toxicity.
2. Data search and selection methods
Articles related to MDMA interactions have been reviewed. The PubMed search included the following keywords and strategies: ‘MDMA OR 3,4-methylenedioxymethamphetamine OR ecstasy,’ AND ‘interaction,’ ‘intoxication’ OR ‘toxicity’ OR ‘death’ OR ‘fatal’ OR ‘adverse drug reaction’ OR ‘drug interaction’ OR ‘polydrug use.’ Only experimental human studies and original data written in English were selected. Related references in relevant articles including reviews and clinical cases were also retrieved.
3. MDMA–drug interactions (MDMA-DIs)
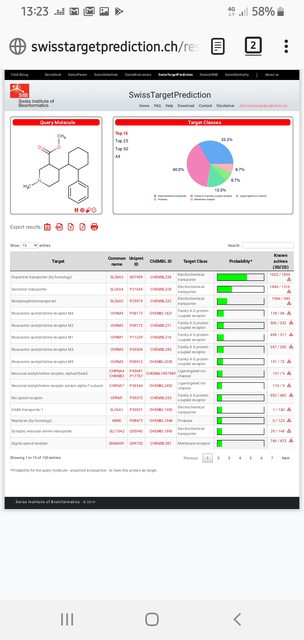
As mentioned, MDMA, as well as other drugs of abuse, is frequently used in combination with other pharmaceuticals and recreational drugs in the same session [83,84]. Considering that MDMA is a potent inhibitor of CYP2D6 substrates, pharmacokinetic, and pharmacodynamic MDMA-DIs can be expected and consequently involved in acute MDMA toxicity [57,58,75–79]. Particularly, the combination of MDMA with other drugs that directly or indirectly affect 5-HT can precipitate a serotoninergic syndrome. According to the literature, it is generally caused mainly by selective serotonin reuptake inhibitors (SSRIs), monoamine oxidase inhibitors (MAOIs) and also by antihistamines (chlorphenamine) and herbal remedies (hypericum or St John’s Wort, ginseng). In this respect, in laboratory conditions, only several experimental clinical studies have evaluated the human pharmacokinetics and pharmacodynamics of MDMA-DIs. An overview of these MDMA-DIs studies mainly conducted for certain pharmaceutical drugs used in psychiatric and other medical conditions (Table 2), as well as drugs of abuse and social drugs (Table 3) is presented.
Table 2. Overview of pharmacokinetic and pharmacodynamic effects of MDMA-DIs with pharmaceuticals.
CSVDisplay Table
Table 3. Overview of pharmacokinetic and pharmacodynamic effects of MDMA-DIs with drugs of abuse.
CSVDisplay Table
3.1. MDMA’s interactions with pharmaceuticals/medicines
3.1.1. Nervous system drugs
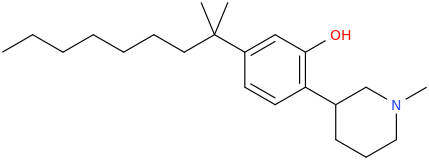
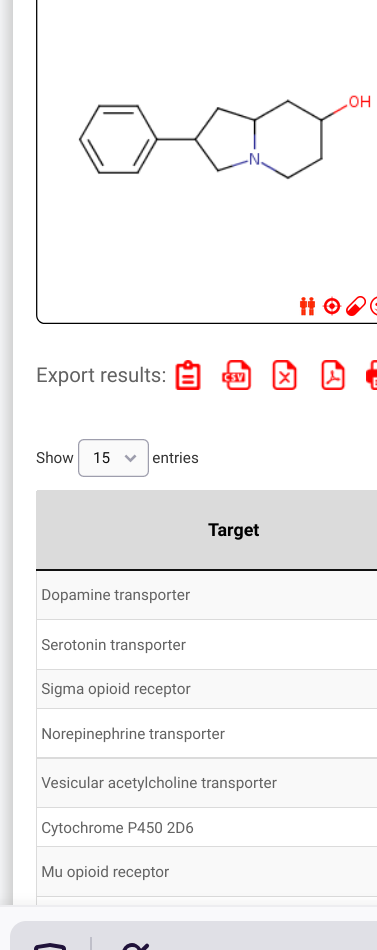
Psychiatric conditions and the recreational use of ecstasy frequently coexist. Antidepressants, antipsychotics, and psychostimulants are used in the treatment of various central nervous system (CNS) disorders, including anxiety-depressive disorders, obsessive-compulsive disorder, psychotic spectrum disorders, and attention-deficit hyperactivity disorder (ADHD). Simultaneously, the use of performance and image-enhancing drugs is a common practice among healthy young people. Because of the CYP2D6 inhibition induced by MDMA, potential DDIs could appear when ingesting prescription drug substrates of CYP2D6. Such substrates include tricyclic antidepressants (amitriptyline, clomipramine, desipramine), serotonin reuptake inhibitor antidepressants (citalopram, fluoxetine, paroxetine), amphetamine-like compounds (methamphetamine), antipsychotics (haloperidol, perphenazine, risperidone), antiarrhythmics (aprindine), antiemetics (dolasetron, ondansetron), beta-adrenoceptor antagonists (alprenolol, metropolol), and opioids (codeine, tramadol).
A total of nine experimental studies have investigated potential MDMA interactions with nervous system drugs in humans.
3.1.1.1. Antidepressant drugs
SSRIs are the most widely prescribed class of antidepressants. SSRIs are potent inhibitors of the metabolism via the CYP450 system and, among them, some have been evaluated in combination with MDMA, such as fluoxetine (a strong inhibitor of CYP2D6 and moderate inhibitor of CYP3A4 and CYP2C9), paroxetine (a very strong CYP2D6 inhibitor), duloxetine (a moderate CYP2D6 inhibitor), while citalopram appears to have little effect on the major CYP isoforms.
The experimental administration of 125 mg of MDMA in healthy subjects that have taken pretreatment with therapeutic doses of paroxetine significantly attenuates MDMA-related physiological and psychological effects [85]. These findings are consistent with the previous administration of intravenous citalopram [86]. The administration of 100 mg of MDMA after 5 days of treatment with therapeutic doses of fluoxetine reduces the MDMA-induced increase in HR without reducing BP [87]. Regarding subjective effects, both studies [85,86] concluded in a significant reduction in prototypical subjective effects and mood subjective effects. MDMA dopamine release mediated by D reuptake inhibition is also amplified through the activation of postsynaptic 5-HT2 receptors [88,89], and they do not exclude the hypothesis of the potential contribution of NE on the subjective effects of psychostimulants such as MDMA [90]. While for the other SSRIs, no pharmacokinetic (PK) interaction was tested, in the case of paroxetine, a significant increase of 30% in MDMA plasmatic concentration was detected along with a decrease of 40% in concentrations of its metabolite HMMA, thus suggesting a pharmacodynamic (PD) (5HT transporter) and also PK (CYP2D6 metabolism) DI [85].
In relation to other types of antidepressants, only three studies have been performed to evaluate the physiological and subjective effects of serotonin-noradrenaline reuptake inhibitors (SNRIs-duloxetine), selective noradrenaline reuptake inhibitors (NRIs-reboxetine) and norepinephrine-dopamine reuptake inhibitors (NDRIs-bupropion) in combination with MDMA [91–93]. In both studies involving duloxetine and reboxetine, pretreatment reduced physiological effects (BP, HR), subjective and mood effects usually produced by MDMA were observed despite 16–20% increase in MDMA plasma concentrations. In the case of bupropion, a known inhibitor of CYP2D6 and CYP2B6/dopamine reuptake inhibitor, it reduced the HR response to MDMA and conversely increased plasma concentrations of MDMA (+15%) and prolonged its subjective effects. Since MDMA is primarily metabolized to HMMA by CYP2D6 [94,95], the effects on the pharmacokinetics interaction are probably explained by CYP2D6 inhibition.
Evidence from experimental studies confirm the existence of a pharmacokinetic interaction mediated by CYP2D6 metabolism between MDMA with antidepressants with CYP2D6 inhibitory actions. Overall, previous administration of all of them produced 15–30% increase of MDMA concentrations, but decreased concentrations of its metabolite HMMA by 40–50% [85,91,92,94]. Thus, the metabolic change and higher MDMA concentrations considered as a phenotyping change from extensive metabolizers (EM) to poor metabolizers (PM) have been observed when antidepressant CYP2D6 inhibitors have been administered before MDMA dosing. In subjects taking medication that inhibits CYP2D6, higher MDMA concentrations and possibly also acute effects should be expected. Contrarily to SSRIs potent inhibitors of CYP2D6, other SSRIs such as citalopram at usual therapeutic dosages are probably less likely to cause significant alterations in CYP450 status and, consequently, have less risk to develop acute toxicity.
3.1.1.2. Antipsychotic drugs
Regarding MDMA-antipsychotic interactions, only one experimental study has been published.
Haloperidol is a typical butyrophenone antipsychotic that exhibits high-affinity dopamine D2 receptor antagonism. In healthy volunteers, pretreatment with haloperidol attenuated MDMA-induced positive and mania-like behavior but had no other effects in reducing subjective changes or cardiovascular effects. Results are consistent with a partial dopaminergic mediation of the euphoriant effects of MDMA [96].
3.1.1.3. Psychostimulant drugs
In relation to MDMA-psychostimulant drug interactions, only one study has evaluated the potential interaction with methylphenidate (MPH) [97].
MPH is a psychostimulant drug prescribed to treat ADHD, a condition that affects around 5% of young people up to 18 years of age worldwide. It is also used for non-medical conditions as cognitive enhancers among healthy subjects.
Pretreatment with MPH produced significantly higher cardiovascular and hemodynamic responses than either drug alone, although pharmacokinetics of MDMA were not altered for MPH administration. MPH did not enhance the psychoactive effects of MDMA. The results observed are in accordance with previous evidences that both drugs induce a weaker increase of NA exerting sympathomimetic properties. MPH mainly enhances DA neurotransmission whereas MDMA mainly acts enhancing 5-HT neurotransmission.
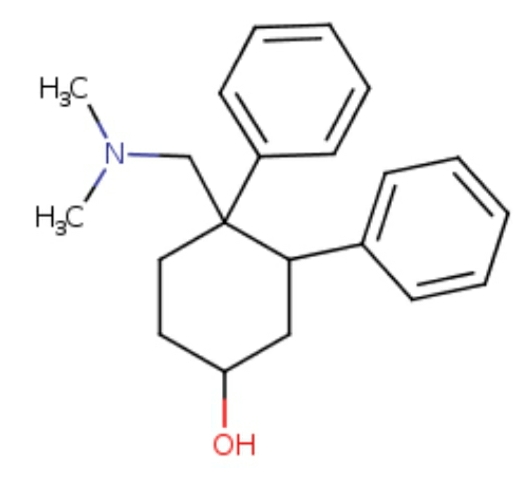
3.1.1.4. Anti-dementia drugs
Memantine is a low-affinity N-methyl-D-aspartate receptor antagonist and alpha 7 nicotinic acetylcholine antagonist approved in some countries for the symptomatic treatment of patients with moderate to severe Alzheimer’s. Memantine has been hypothesized as a potential drug to prevent and/or overcome the memory impairment caused by MDMA use in humans. In fact, some ecstasy drug-user forums and blogs reported MDMA use in combination with memantine to provide neuroprotection and to reverse deficits in learning/memory.
In this respect, only one experimental study has been performed in humans in order to evaluate MDMA–memantine interaction, which had negative results. Preliminary evidence shows that memantine does not reverse MDMA-induced memory impairment and mood effects. In addition, no PK changes were detected in MDMA concentrations [98].
3.1.2. Cardiovascular system drugs
As previously mentioned, acute exposure to MDMA has been described to produce profound cardiostimulant and thermogenic effects that, in cases of severe MDMA toxicity (tachycardia and hyperthermia), may result in multiorgan failure associated to heatstroke. In clinical practice, both HR and T increases are easily detectable and noninvasive markers of the severity of the MDMA intoxication. Probably for these reasons, the potential interaction between certain cardiovascular drugs and MDMA has been experimentally investigated.
3.1.2.1. Beta-adrenergic antagonists (β -blockers)
Pindolol is a nonselective beta-adrenergic antagonist (beta-blocker) used as an antihypertensive agent. Pretreatment with pindolol reduced MDMA-induced tachycardia but reduced neither hypertensive effects nor other adverse effects related to MDMA [99]. Furthermore, while pindolol moderately attenuated the increases in positive mood, dreaminess, derealization, and mania-like behavior induced by MDMA, it did not have any effect on MDMA-induced cognitive performance impairment. These results could be attributed to a potential role for serotonergic 5-HT1 receptors in the mediation of the mood effects of MDMA [100].
3.1.2.2. Βeta1 (β1) and alfa1 (α1) adrenergic antagonist/nonselective β-adrenoreceptor (mixed blockers)
Carvedilol is an alfa1 (α1) and beta (β1) adrenergic antagonist indicated for the treatment of mild-to-severe chronic heart failure of ischemic or cardiomyopathic origin, usually in addition to diuretics, angiotensin-converting-enzyme inhibitors (ACE inhibitors), and digitalis. Probably, based on the evidence of the beta-blocker effect of the cocaine-induced hemodynamic response in humans, the potential existence of an interaction between carvedilol and MDMA has been evaluated. Pretreatment with carvedilol reduced MDMA-induced increases in BP, HR, and T, although it did not affect the subjective effects of MDMA neither did it modify the MDMA plasma concentrations [101].
3.1.2.3. Alfa2 (α2) adrenergic agonist
Clonidine is an α2-adrenergic agonist used as an antihypertensive agent. Pretreatment with clonidine modified neither the physiological nor the subjective effects. No alteration was detected in plasma concentrations of MDMA. The coadministration of MDMA and clonidine results in a decrease in plasma concentration of NE, which has been correlated with hypotensive effects [102].
3.1.2.4. Alfa1 (α1) adrenergic antagonist
Doxazosin is an α1-adrenergic antagonist used to treat hypertension and symptoms of benign prostatic hyperplasia. Pretreatment with doxazosin had very modest effects on HR and BP produced by MDMA but not on T. Doxazosin has been proven to attenuate the mood effects of MDMA [103]. As expected, the effects of doxazosin on the cardiovascular response of MDMA are consistent with the sympathetic effects mediated by the effects of epinephrine and NE on peripheral vasculature.
3.1.2.5. Ketanserin 5-HT2A/C antagonist
Ketanserin is a 5-HT receptor antagonist antihypertensive drug, as well as an adrenergic receptor blocker, and dopamine antagonist. The experimental administration of MDMA in pretreatment with ketanserin produced a reduction in anxiety but not in memory test scores. In addition, no alterations in MDMA concentrations were observed [100,104,105]. Ketanserin attenuated MDMA-induced perceptual changes, emotional excitation, and acute adverse responses [106]. Evidence shows that 5-HT1 and 5-HT2 receptors contribute to the influence of MDMA on mood and impulsivity.
3.1.3. Cough and cold preparations
Dextromethorphan (DEX) is an over-the-counter (OTC) antitussive found alone and in most cough and cold products, frequently in combination with antihistamines and/or pseudoephedrine. DM has a complex pharmacology with mechanisms beyond blockade of N-methyl-d-aspartate (NMDA) receptors and inhibition of glutamate excitotoxicity, likely contributing to its pharmacological activity and clinical potential. It is well knowledged that DEX is primarily metabolized to dextrorphan by CYP2D6, which has hampered the exploration of DEX therapy separate from its metabolites [107].
DEX has been used as a probe drug to evaluate changes in CYP2D6 activity using the urinary metabolic ratio of DEX and dextrorphan [16,108]. MDMA administration before DEX produced a strong inhibition of CYP2D6 that reduced the metabolism of DEX, recovery to 90-100% last 10 days after MDMA exposure in both men and women. Based on these findings, MDMA-induced mechanism-based inhibition was confirmed.
3.2. MDMA-DIs with drugs of abuse or social drugs
Data in humans regarding scientific information about the interaction of MDMA with drugs of abuse or social drugs is very limited. The unique experimental studies of the interaction between MDMA have been performed with alcohol and cannabis (tetrahydrocannabinol-THC), the two most common drugs of abuse (legal or illegal) used with recreational and caffeine used with social purposes in the world. There are no studies in humans evaluating potential interaction between MDMA in combination with other popular drugs used alongside MDMA such as cocaine, opioids, lysergic acid diethylamide (LSD), GHB, ketamine, sildenafil, or NPS among other ones. The reason for the lack of human scientific data is unknown [108,109]
3.2.1. MDMA
The effects of MDMA-MDMAIs have been of special interest due to the common practice among recreational ecstasy/MDMA users of repeated MDMA doses in the same session, as well as life-threatening and fatal cases of acute MDMA toxicity after high and repeated MDMA doses. The number of pills administered in the same session varies from 0.5 to 5 pills, with total doses varying from 50 mg to 300 mg [110]. Three clinical trials have administrated different doses used for recreational purposes (50 mg, 100 mg) with different intervals of administration (2 h, 4 h, and 24 h) [110–113]. All of them have demonstrated a phenomenon of MDMA accumulation after the second dose. In all of them, higher MDMA plasma concentrations were detected but had lower acute effects than expected. Following a second MDMA dose, MDMA Cmax increased +18% at 2 h (50 + 100 mg), +23.1% (100 + 100 mg), and 29% at 24 h (100 + 100 mg), whilst for the metabolite HMMA, after the second dose, it showed lower concentrations – Cmax decreased −38.2% and −43.3% at 2 h and 4 h, respectively. These changes in MDMA and HMMA concentrations have been explained as a consequence of a CYP2D6 metabolic auto-inhibition that lasts over the activity of CYP2D6, which recovered after 10 days with a recovery half-life of 48 h [16,111–113]. After the second MDMA dose, the pharmacological MDMA effects produced were similar or slightly greater than those of the first one. The results consistent with increases in MDMA concentration not related to acute MDMA effects have been postulated as a phenotype change from EM/intermediate metabolizers (IM) to PM and a possible acute tolerance phenomenon, respectively.
The other two studies have evaluated the effects of repeated MDMA doses (75 mg and 50 mg separated by 4 h) on memory, mood, impulsivity, and psychomotor performance [114,115]. As expected, sleep deprivation irrespective of drug/placebo administration produced a deterioration of memory and psychomotor tasks. Under the influence of consecutive MDMA doses, in addition to the effects induced by sleep loss throughout the night, MDMA produced an impairment of tracking performance (divided attention and memory, both verbal and spatial), increased subjective effects and decreased sleepiness scores.
3.2.2. Alcohol
Alcohol is the most widely used licit substance worldwide and the mainly concomitant substance used among ecstasy/MDMA users. It is a CNS depressant drug that promotes simultaneous changes in several neuronal pathways that lead to various behavioral and biological alterations. Alcohol exerts direct effects on several neurotransmitter receptors (gamma-aminobutyric acid [GABA], glutamate, endocannabinoids, and others), indirect effects on the limbic and opioid systems, and also effects on calcium and potassium channels and on proteins regulated by GABA in the hippocampus [116]. Four studies in experimental conditions point out that concomitant MDMA and alcohol produce an increase of MDMA concentrations ranging from 7% to 13% and long-lasting duration of subjective effects [117–121]. Unpublished data of the same study [111] showed that the combination produced higher and long-lasting cardiovascular effects (BP and HR) and a slight increase in body temperature. The use of both drugs increases the levels of DA in the brain due to dopamine’s function in the experience of reinforcement. The euphoria that occurs as a result of these drugs is reinforcing, which leads to an increase in DA.
3.2.3. Cannabis (THC)
Cannabis (THC) is a drug of abuse frequently used among recreational ecstasy/MDMA users to reduce MDMA’s initial psychostimulant effects and to attenuate the post-MDMA comedown. Preclinical studies have shown that a combined administration of MDMA with THC induces hyperthermia and decreases hyperactivity in animal models in order to achieve neuroprotection and/or prevent toxicity [122]. In humans, the investigation in experimental conditions is limited to one clinical trial [123]. Results did not show alterations in MDMA plasma concentrations, but they did show a significant reduction in HR.
3.2.4. Caffeine
Caffeine (1,3,7-trimethylxanthine) is the most consumed legal psychoactive substance contained in foods and beverages such as coffee, sodas, energy drinks, and shot energy among others in the world. It acts on adenosine receptor as antagonism whose actions include G-protein-coupled mainly. It exerts CNS effects mainly by antagonizing the adenosine A1 and A2A receptors [124]. It is commonly used in combination with MDMA in order to reduce drowsiness and fatigue primarily as energy drinks and caffeine tablets and more recently as caffeine intranasal sprays and sublingual strips [125,126]. It is notable to remark that caffeine is also present as an adulterant in ecstasy pills [67,127]. Caffeine, similarly to DEX, has been extensively used as a probe drug to investigate CYP1A2 activity, based on the ratio of caffeine and its metabolite paraxanthine. There is only one study has monitored caffeine metabolism by CYP1A2 after MDMA administration. The results showed a modest increase in the metabolism of caffeine. In terms of CYP1A2 activity, the results shown an increase in activity when CYP2D6 is inhibited by MDMA in both genders, being more pronounced in females. It points out the existence of a compensatory mechanism between the CYP 450 isozymes in order to metabolically clear MDMA [128].
4. Conclusion
Scientific evidence provides some insight into potentially significant MDMA-DIs with pharmaceuticals and other drugs of abuse. It is important to understand the implications of these interactions to reduce the risk of acute MDMA toxicity. It is essential to take into consideration the fact that MDMA-DIs including MDMA-MDMAIs vary for each subject because of multiple conditions (environmental and individual genetic variability). Despite the widespread use of MDMA in combination with pharmaceuticals and drugs of abuse (polydrug use), substantial deficiencies remain regarding the potential MDMA-DIs. Definitely, more systematic investigation focused on better understanding MDMA-DIs acute pharmacological effects and toxicity in humans are warranted.
5. Expert opinion
Despite the extended recreational use of MDMA/ecstasy in combination with pharmaceuticals and drugs of abuse for over decades, there is a reduced number of published MDMA-DIs studies and scarce clinically significant MDMA-DIs documented in the literature. The present review emphasizes the potential MDMA-DIs that can lead to clinically relevant interactions and serious acute toxicity. It is important to keep in mind that there is not a specific treatment for acute MDMA intoxication – it varies from the initial management and assessment to the supportive care of severe symptoms, and especially MDMA-DIs suppose a more complex challenge.
To date, although several published reports appear to indicate the importance of polydrug use among ecstasy/MDMA recreational users, only few human studies have experimentally investigated potential PK and PD MDMA-DIs. Nevertheless, based on these limited scientific data available from experimental MDMA-DIs studies, some general recommendations should be considered in relation to the use of MDMA in combination with certain pharmaceuticals and drugs of abuse.
Evidence indicates that MDMA is metabolized mainly by CYP2D6, suggesting that inhibitors of this hepatic isozyme could potentially result in altered MDMA PK parameters. These results are in accordance with findings described on clinical cases’ reports in which CYP2D6 inhibitors have been documented as the main cause of life-threatening interactions with MDMA (Papaseit et al. 2015; Henry et al., 1998), as well as multiple cases of suspected acute MDMA/ecstasy interaction with CYP2D6 inhibitor drugs (no toxicological analysis results). MDMA as a potent CYP2D6 inhibitor can reduce the metabolism of a number of drugs that are cleared by this cytochrome.
Limited data suggest that cardiovascular drugs, mainly antihypertensive, in combination with MDMA do not have significant effects on MDMA concentrations, neither do they have clinically relevant effects.
As mentioned, one of the most important concerns is the concurrent use of MDMA with other drugs of abuse, which yet continues to be controversial due to reports of acute intoxications and few experimental MDMA-DIs studies performed. The potential for MDMA interaction exists when it is co-administered with other psychostimulants. Whilst for MDMA and classical drugs of abuse acting on the central nervous system potential pharmacokinetic/pharmacodynamic (PK/PD) interactions can be more easily anticipated, the combination of MDMA with NPS is a non-explored area difficult to predict. Finally, MDMA-MDMAIs are the best well-known source of potential toxicity that could lead to clinically relevant interactions and serious intoxications.
Anyway, all these findings have been obtained in unique experimental MDMA-DIs studies with optimal conditions and, consequently, need to be very prudently extrapolated to practice. In this context, it is very crucial that clinicians and health-care providers be informed in relation to the potential MDMA-DIs with pharmaceuticals and also with drugs of abuse. As with other DDIs, it is imperative that clinical assessment of MDMA-DIs considers coexisting medical diseases and other specific information/factors (sex-gender, race-ethnicity, genetic polymorphism) to determine the real risk of potential PD and/or PK interactions. Regardless of this, it is important to be aware of the new use of pharmaceuticals (cognitive, performance and/or image-enhancing drugs) as well as the ever-changing map of NPS, in which cases there are no data in relation to potential interactions. Besides, knowledge of MDMA-DIs will be essential if MDMA-assisted psychotherapy is consolidated as a treatment for post-traumatic stress disorder, social anxiety in autism, anxiety associated with life-threatening illness and/or alcohol use disorder. Finally, continued research on this topic is highly warranted.
Article highlights
The knowledge of potential MDMA-DIs is crucial to minimize acute potential MDMA toxicity.
Polydrug use in recreational ecstasy/MDMA users, including pharmaceuticals and drugs of abuse, is an added risk factor that can lead to MDMA-DIs and it represents an important source of related medical emergencies and even fatalities.
Most relevant documented MDMA-DIs from experimental evidence show a pharmacokinetic interaction mediated by CYP2D6 with antidepressants with CYP2D6 inhibitory action.
Most clinically relevant MDMA-DIs are consistent with mechanism-based inhibition of CYP2D6 by coadministration of CYP2D6 inhibitors (including pharmaceuticals and MDMA).
Repeated use of MDMA (MDMA-MDMAIs) is a relevant MDMA-DI which should be considered in order to minimize potential acute toxicity.
MDMA-DIs are a complicated clinical entity that involve, in addition to the very interaction factors, other determinants to be considered (sex-gender, race-ethnicity, genetic polymorphism …), which makes them unpredictable.
The lack of scientific knowledge concerning MDMA-DIs with the most used pharmaceuticals and drugs of abuse is highlighted.
This box summarizes key points contained in the article.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
This work was supported in part by grants from Instituto de Salud Carlos III (ISCIII, FIS-FEDER, FIS-PI17/01962), the ISCIII-Red de TrastornosAdictivos (RTA RD16/0017/003 and RD16/0017/0010), and Suport Grups de Recerca AGAUR-Gencat (2017 SGR 316 and 2017 SGR 530). Esther Papaseit is a Juan Rodés fellowship (ISC-III, JR16/00020).
References
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.