mr peabody
Bluelight Crew
- Joined
- Aug 31, 2016
- Messages
- 5,714

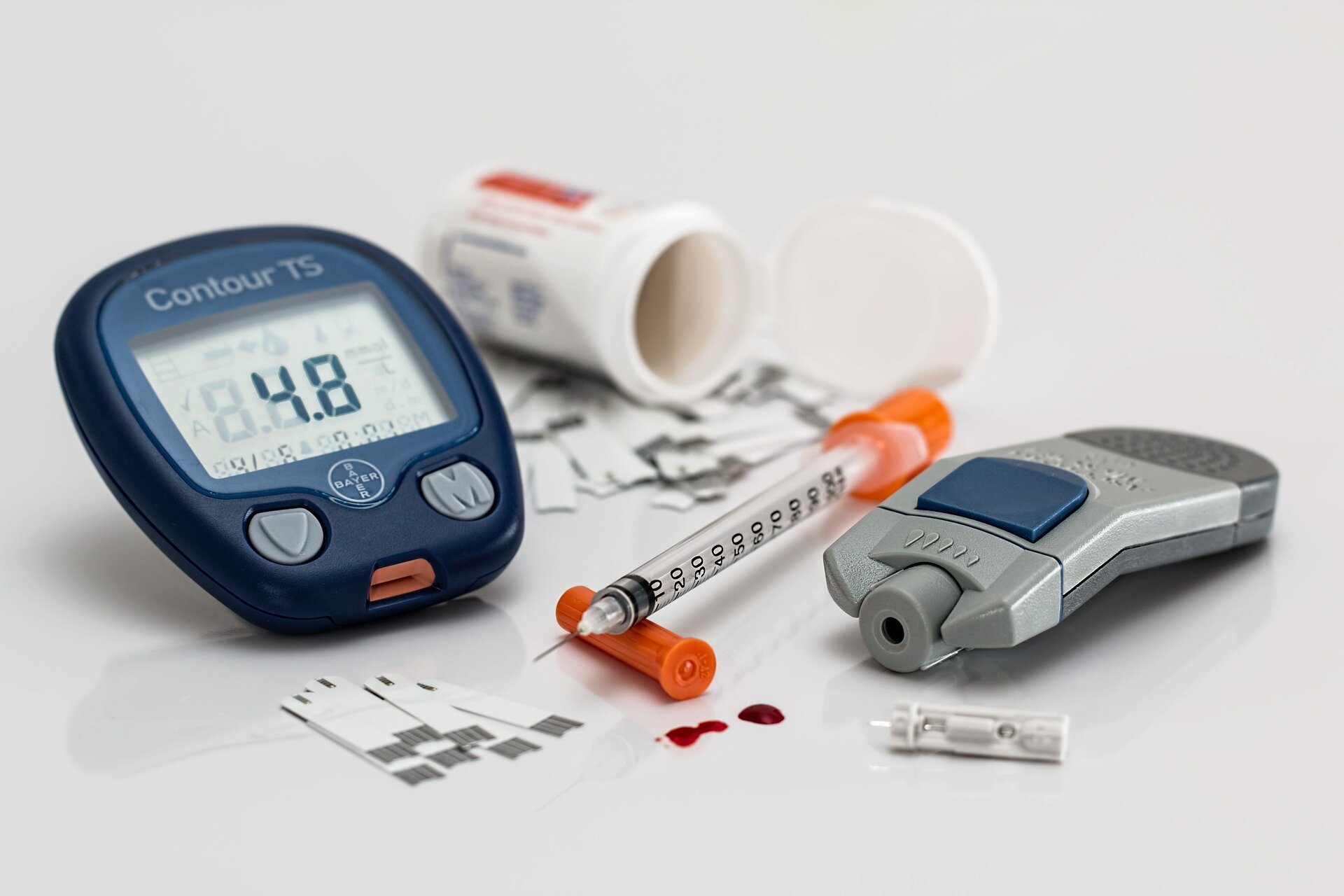
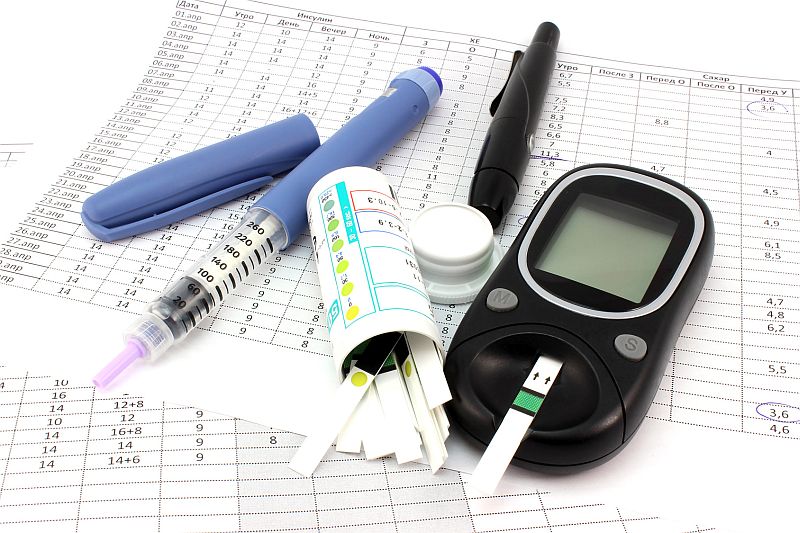
Self-adjusting insulin promises safer blood sugar control of Diabetes
by Rich Haridy | NEW ATLAS | 3 December 2020
An incredible proof-of-concept study from a team of European scientists has demonstrated the development of a novel insulin molecule that can sense blood sugar levels and self-adjust its activity in response to a patient’s needs. The experimental molecule has only been tested in animals so far but the researchers are hopeful further development will offer diabetics a safer and easier insulin therapy in the future.
For most diabetics, maintaining healthy blood sugar levels is akin to constantly balancing on a tightrope. Insulin injections can help lower high blood sugar, but too much insulin or dosing at the wrong time can be dangerous, leading to hypoglycemia.
"The difficult thing with diabetes is that insulin always works the same way,” explains Knud Jensen, an author on the new research from the University of Copenhagen. “It lowers blood sugar, even though that might not be what a patient requires.”
Jensen says he was compelled to develop a safer form of insulin after a colleague told him a story years ago of a type 1 diabetic who passed away after his wife mistakenly gave him insulin at the wrong time. The man was feeling unwell and, thinking it was the result of high blood sugar, insulin was administered. But sadly, the dose of insulin ultimately led to the man’s death.
"That is why we have developed the first step towards a kind of insulin that can self-adjust according to a patient’s blood sugar level,” says Jensen. “This has tremendous potential to vastly improve the lives of people with type 1 diabetes.”
The impressive research presents a novel glucose-responsive insulin molecule that can spontaneously increase, or decrease, its activity in response to circulating blood sugar levels.
"The molecule constantly releases a small amount of insulin, but varies according to need," says Jensen. “It will give type 1 diabetes patients a safer and easier treatment.”
The new study not only describes the development of this novel insulin molecule but demonstrates its efficacy in animal models. The unprecedented experiments show the insulin effectively responding to blood glucose fluctuations in rats.
Jensen is optimistic about his team’s achievement but pragmatically notes there is still years of work ahead before this kind of self-regulating insulin hits the market. The research is still in the preliminary stages and it hasn't yet been demonstrated to be safe or effective in humans. However, this is still a landmark achievement in chemistry, offering the first evidence of a glucose-responsive insulin molecule working in a live organism.
"We've tested the insulin molecule on rats and it has proven itself effective,” says Jensen. “The next step is to develop the molecule so that it works more rapidly and accurately. And finally, to test it in humans – a process that can take many years. But it is certainly worth pinning one’s hopes on.”
The new study was published in Chemistry, A European Journal.
Source: University of Copenhagen

Self-adjusting insulin promises safer blood sugar control for diabetics
An incredible proof-of-concept study from a team of European scientists has demonstrated the development of a novel insulin molecule that can sense blood sugar levels and self-adjust its activity in response to a patient’s needs. The experimental molecule has only been tested in animals so far but…
Last edited: