My experience with ketamine therapy for depression
@Foreigner's great report from 2013 (chapters 1-5)
I’ll be using this thread to talk about my use of low-dose ketamine as a mental health aid, specifically for chronic depression that has never been really cured with conventional treatment.
My inspiration comes partly from Jamshyd’s Ketamine Regimen, but I did not attach my report to his thread because there are going to be some divergences in opinion, plus I just have a lot to say and I’d like to be thorough.
I originally was not going to write a report on this but in reflecting upon my own struggle with trying to get more precise information about how to carry out this regimen, I believe my input would help someone out there who might have already been considering this approach but is going through a similar challenge. Also, I feel there is just not enough first-person reporting on this regimen to coincide with the research findings, and it's a gap I would like to contribute to filling.
Most importantly, this regimen appears to have worked for me, and I believe that seed of truth deserves to shine somewhere.
Disclaimer
Although I am trained in the scientific method, this work was not carried out in a professional setting. Please keep in mind that this regimen remains controversial. Although NMDA antagonists offer a wealth of promise for the future treatment of depression and other mental health issues, most sources admit that ketamine is a rather raw and unrefined approach for this purpose, and is being employed until better alternatives can be developed. You should therefore not be considering this regimen unless the conventional approaches have all failed.
Another warning I must give – probably more important than the above – is that this regimen is for those who embody the utmost self-discipline. Ketamine’s euphoric and transcendent properties make it a substance easily abused. Even in a low-dose regimen, the temptation to do “just a little more this dose” can be ever present. Each brief period of euphoria makes you feel as though you are close to a supreme truth, if only you could do just a little more to figure it out. Do not chase this feeling, it is a transient, false lure. If you can avoid the pitfalls by always sticking to the allotted dose, this regimen could very well work for you. For those who lack the discipline, I believe a clinical setting where someone else controls the allotment would be more ideal.
Side effects
Ketamine is not without its side effects, and this is not a perfect therapy, even for someone like me who is in a state of finely tuned health. (For more details, see the section on "negative effects" below.)
Because I am an eastern medicine practitioner, I am able to pick up on subtle signs of physiological changes more readily than the more obvious western diagnostic signs. From day one there were impacts to the kidneys and urinary system. Urine was darker no matter how much I hydrated, and there was usually floating matter in the urine. There was minor kidney colic as well as spasm of the kidney meridian down the inside of the legs. My kidneys were in a constant state of trying to purge, including at night time when I was awoken repeatedly to urinate. I had minor lower back pain (also a kidney sign).
Liver and gallbladder both took a hit too. The constant bitter taste in my mouth, red and dry eyes, and systemic sluggishness due to processing metabolites, were not major, but still noteworthy.
I’m prone to insomnia and ketamine made it much worse. My sleeping schedule was basically in chaos for most of the time and I slept at all random hours on the 24 hour clock. But then, this happens to me when I take most drugs, even cannabis. If you are prone to insomnia I strongly urge you to approach this regimen with caution, but with that said, this might actually help your sleep for all I know.
Though the evidence remains inconclusive, there is the uncharted risk of Olney’s lesions in the brain. This is admittedly due to higher doses of ketamine and regular abuse. I personally believe that the risk is unfounded but it’s one that prospective users of this regimen should know about. Interestingly, Jamshyd mentioned that using gabapentin in combination with this therapy helped him a great deal. This link states that, "In medical settings, NMDA receptor antagonists are used as anaesthetics, so GABA-A receptor positive allosteric modulators are used to effectively prevent any neurotoxicity caused by them." This could suggest that any potential toxicity of ketamine could be at least partially mitigated by gabapentin, though I did not use it so I cannot comment.
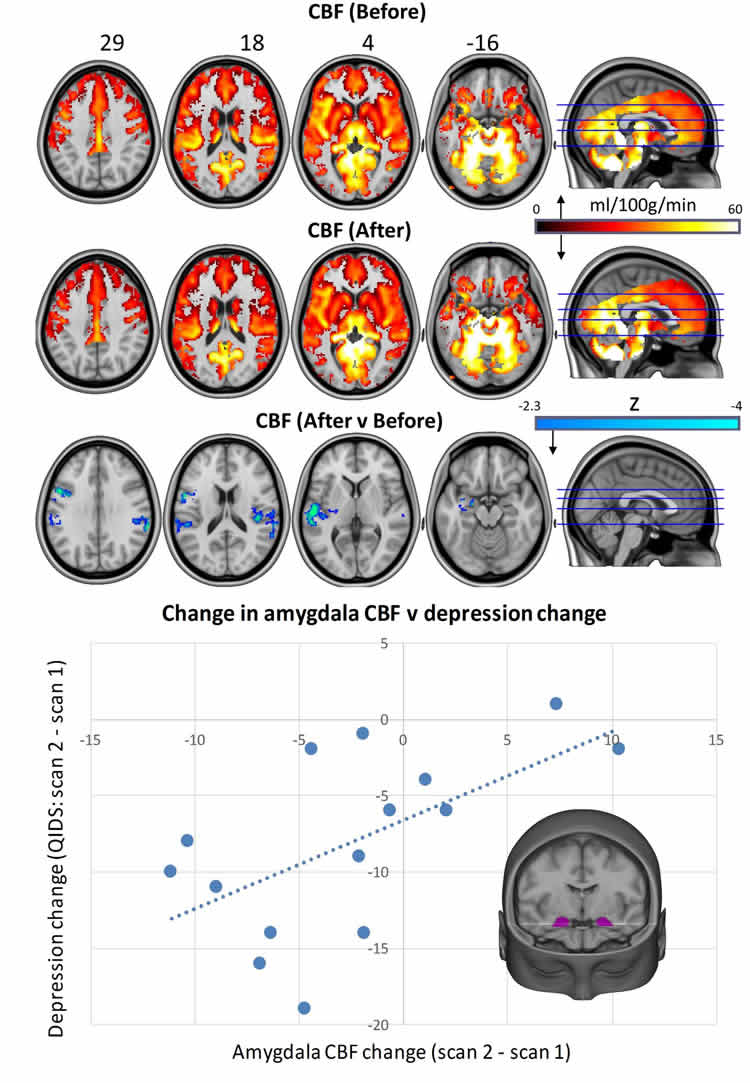
The science
The empirical evidence behind ketamine being an effective diffuser of depressive and suicidal states has already been explored relatively thoroughly in Jamshyd’s thread. I will however add these summary links for further reading:
http://www.sciencedaily.com/releases...0819141913.htm
http://www.sciencedaily.com/releases...1004141747.htm
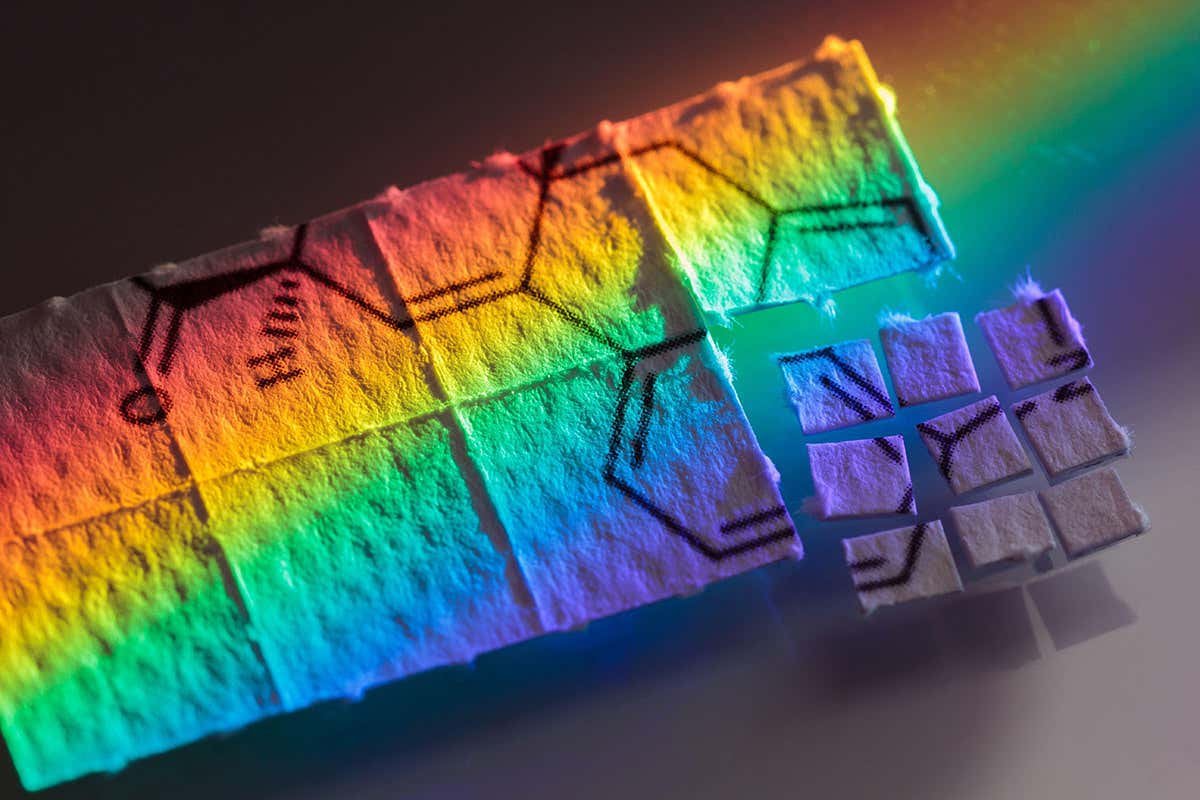
In most of the clinical research they administered single larger doses, which usually resulted in temporary depression relief for up to 7-10 days. The regimen I am using, modelled after Jamshyd’s, is based on the hypothesis that ultra low, frequent dosing could have a more cumulative nootropic effect on the NMDA system and therefore could result in longer lasting relief, as well as actual regeneration of synaptic tissue.
A slow release transdermal patch would work great for ketamine. I came across reports of some hospitals using these for post-operative pain in gynecological procedures, but it was formulated to work locally and not pass the blood brain barrier. Since the pharmaceutical industry is hard at work making non-psychedelic NMDA medications, don’t expect a ketamine patch for depression to happen anytime soon.
Why I chose to do this
A combination of reasons really. One reason is that I anecdotally noticed being in a better mood after a brief stint of recreational ketamine use almost 10 years ago, and that already got me thinking about it. The main reason though is that my unusual metabolism means I process most oral pharmaceuticals irregularly from the established norms. I either suffer rarer side effects or I have no effects at all. SSRIs have proven to be of limited value to me. Ketamine’s rapid action means I would have to endure side effects for less time if the medicine ends up working, and its injectable form means I can bypass the limitations of the digestive route.
Additionally, I’ve long since had the perception that trauma after trauma in my life has caused unfavourable neurological and personality changes, combined with past heavy drug abuse with MDMA, and these are all aspects which talk therapy and conventional pharmaceuticals have never seemed to help me recover from. Eventually there comes a time when you've talked until the cows came home and you still feel unfulfilled; and sometimes, it really
is just a neurochemical imbalance and there is nothing outwardly the matter anymore. I would describe myself this way.
For a very long time there has been that missing link - something in my mind that feels blocked, unable to be overcome or bypassed. It's not necessarily about logic, but it has felt like a deficit. Now the science about PTSD is more clear on this, but effective reparative alternatives are either still under development or simply not being offered. If there is any remote chance that low-dose ketamine could act as a regenerative nootropic to years of traumatic down-regulation, it’s a chance I’m willing to take.
Last but not least, I needed a medicine that has a psychoactive component in order to connect psychospiritually to the process, which is the opposite of the emotionally deadening effects that conventional anti-depressants sometimes induce. Without this necessary quality, no therapy can work for me. I’m of the opinion that modern medicine should not be trying so hard to demonize “euphoria” as an unwanted side effect of medication, as bliss can be a useful healing tool in the right context.
Preparation advice
I only acquired 1g of pure ketamine, more than enough to last for one cycle of this regimen. Though I am not prone to addiction, the choice to not purchase more was a precautionary measure to prevent abuse.
I advise anyone doing this procedure to do the same. Even if you decide to do a second cycle of treatment, just acquire the additional amount at that time, and not in advance.
I recommend titrating your solution so that you are only administering 0.5cc per dose because I found regular injections of bacteriostatic solution (plus the ketamine itself) to be dehydrating and imbalancing to the electrolytes of my body.
I timed this regimen during a period when I would be off work and free of the usual daily obligations. I let my closest and most supportive friends know what I was about to do, both because I planned to still spend time with them while there was ketamine in my system, and because I wanted them to observe me for positive or negative personality changes. (Hey, sometimes it’s possible to go off the deep end and not realize it!) I also made sure the fridge was stocked so that going outside was optional, and had a good playlist of tunes at the ready in case silence became a burden.
Basically, try to make life as materially easy on yourself as you can. During this period of neuroplasticity, you don’t want to be bogged down with run of the mill minutiae. Treat this as therapy and build your healing container accordingly.
In my case I decided that a healthy balance between social time and alone time were necessary. Exposure to the outside world allowed me to alter my approaches and reactions to many different situations, at will, thanks to the enhanced novelty effect. (More on this later.) Being with friends helped me to expand the pallet of venues and events that I could practice new ways of being in. Then, being alone allowed time for deep reflection, inner processing, and connecting with whatever was surfacing. Even at low doses, I would not recommend isolating oneself as dissociatives can be illusory.
I do believe that ketamine in of itself relieves the symptoms of depression, but perhaps more crucially than that, it offers the opportunity for you to explore the root of it. You can just sit there and do nothing while the biochemistry does some of the work for you, or you can go a bit further and delve into your own psyche. The choice is yours.
Continued here:
http://www.bluelight.org/vb/threads/669468-Experience-with-ketamine-therapy-for-depression