Beating prostate cancer with cannabis oil
by Dennis Hill, Biochemist
3 years ago, after a prostate biopsy, I received the diagnosis of aggressive Stage III adenocarcinoma. I didn't know what to do. The urologist made appointments for me to start radiation, and maybe chemo. Then a friend told me cannabis cures cancer. It just so happened that the first human trials of cannabis treatment of astrocytomas (inoperable brain cancer), were published with encouraging results. So I decided; rather than die from the medical treatment, I would do the cannabis cure. Now, where to get some. There was no dispensary in the area, but a friend made me cannabis butter, so I took that, up to tolerance. In 3 months the primary cancer was gone, only minor metastatic lesions were left. After that I found a supplier for Rick Simpson oil and killed off the metastases in the next 3 months. Now I just take a maintenance dose of locally produced hash oil that is 1:1 THC:CBD with about a 30% potency. This will certainly keep me clear of cancer, anywhere, forever.
My point in telling this story is that in the face of advanced aggressive cancer, all I had was very weak cannabutter, but it was enough to eliminate the primary tumor. Now there are strains of 95% THC. But is this necessary? If you have cancer and want to pursue the cannabis treatment, any at all will be good. More important than extreme potency, is balance between THC and CBD. If you can get high potency, great. If not, common potencies will work perfectly.
Finally, if you choose cannabinoid treatment, start small, then increase dosage as rapidly as tolerable. To kill cancer you have to hit it hard, be conscientious about your treatment. Cannabis does no harm to the body, it is a metabolic support for the immune system.
The alternative
As the body, its organs and tissues, fall out of balance or become diseased, cannabinoids have a restorative effect wherever the tissues are damaged, bringing optimal health in all structures and functions. To illustrate this, one particular cannabinoid detects proliferation of tumor cells, binds to the appropriate receptor site (CB2), and causes cancer cell death, leaving normal cells untouched. This effect is shown easily in the lab, but is this scalable to the human condition? We shall see.
In my high school physiology course, the first important concept I learned was homeostasis, the persistent tendency of the body to maintain metabolic balance. It does this through several related systems; so we see that the body likes to be healthy and happy. That is its nature.
Why does the body allow these foreign cannabinoids to come in and take control of such essential physiological processes, without some kind of reaction? It is simply because this modulation system is already set up, and has been functional for millions of years; it's in the DNA of all living creatures. Only it's called the endocannabinoid system. Let's look and see what this system is all about. In the Journal of Neuroimmunology we find a succinct summary:
The endocannabinoid system consists of cannabinoid receptors, their endogenous ligands and enzymes for synthesis and degradation of endocannabinoids and represents a local messenger system within and between the nervous and immune system. Apparently, the endocannabinoid system is involved in immune control and neuroprotection.
This is amazing. Our own endocannabinoid system covers all cells and nerves; it is the messenger of information flowing between our immune system and the central nervous system (CNS). It is responsible for neuroprotection, and micro-manages the immune system. This is the primary control system that maintains homeostasis; our well being.
Just out of curiosity, how does the work get done at the cellular level, and where does the body make the endocannabinoids? Here is a quick look:
In standard neurotransmission, the pre-synaptic neuron releases neurotransmitter into the synaptic cleft which binds to cognate receptors expressed on the post-synaptic neuron. Upon binding, the neuron depolarizes. This depolarization facilitates the influx of calcium into the neuron; this increase in calcium activates an enzyme called transacylase which catalyzes the first step of endocannabinoid biosynthesis.
Here we see that endocannabinoids have their origin in nerve cells right at the synapse. When the body is compromised through illness or injury it calls insistently to the endocannabinoid system to direct the immune system to bring healing. If these homeostatic systems are weakened, it should be no surprise that hemp cannabinoids are therapeutic. It helps the body in the most natural way possible.
The endocannabinoid system
To see how this works we visualize the cannabinoid as a 3-dimensional molecule, where one part of the molecule is configured to fit the nerve or immune cell receptor site just like a key in a lock. There are at least two types of cannabinoid receptor sites, CB1 (CNS) and CB2 (immune). In general CB1 gives us the buzz, and CB2 activates the immune system, but it's much more complex than this. Both THC and anandamide activate both receptor sites. Other cannabinoids activate one or the other receptor sites. Among the strains of Cannabis, C. sativa tends toward the CB1 receptor, and C. indica tends toward CB2. So sativa is better for buzz, and indica is better for healing. Another factor here is that sativa is dominated by THC cannabinoids, and indica is predominately CBD (cannabidiol).
It is known that THC and CBD are biomimetic to anandamide, that is, the body can use both interchangeably. Thus, when stress, injury, or illness demand more from endogenous anandamide than can be produced by the body, its mimetic exocannabinoids can be administered. If the stress is transitory, then the treatment can be transitory. If the demand is sustained, such as in cancer, then treatment needs to provide sustained pressure of the modulating agent on the homeostatic systems. This is why Rick Simpson recommends twice daily doses of hemp oil extract (C. indica), for three months, in the case of cancer.
Typically CBD gravitates to the densely packed CB2 receptors in the spleen, home to the body's immune system. From there, immune cells seek out and destroy cancer cells. Interestingly, it has been shown that CBD cannabinoids have the ability to kill cancer cells directly without going through immune intermediaries. CBD hijacks the lipoxygenase pathway to directly inhibit tumor growth. As a side note, it has been discovered that CBD inhibits anandamide reuptake. This means that cannabidiol helps the body preserve its own natural endocannabinoid by inhibiting the enzyme that breaks down anandamide.
Coincidentally, it is not only CBD that is specifically cytotoxic to cancer cells, THC takes a different approach the task:
THC achieves this wizardry by binding to protein receptors on a cancerous cell?s surface. Once attached, the THC induces the cell to make a fatty substance called ceramide, which prompts the cell to start devouring itself. We see programmed cell death. What's more, noncancerous cells don't make ceramide when they come into contact with THC. The healthy cells don't die.
Just for clarity, endogenous ceramide (a signaling sphingolipid) disrupts the mitochondrial function of making ATP (adenosine triphosphate), thus the cancer cell becomes energy starved. ATP is the energy donor for all essential cell functions. Once the mitochondria shut down, the cell dies.
Endogenous ceramide's day job is to speed destruction of already stressed or senescent cells. We seen now that in the presence of THC, ceramide senses cancer cells as stressed or senescent, thus speeding their death.
Before leaving this topic it is important that we differentiate between plant based ceramide (phytosphingosine) and mammalian ceramide (endogenous sphignosine). Plant ceramide has a slightly different molecular structure but very different bioactivity. Ingested, it is a moisturizing lipid that supports the skin (stratum corneum) enhancing the moisture barrier that keeps epidermis from drying out. This is good, you should get some. I tried it and liked it.
How cannabis oil works
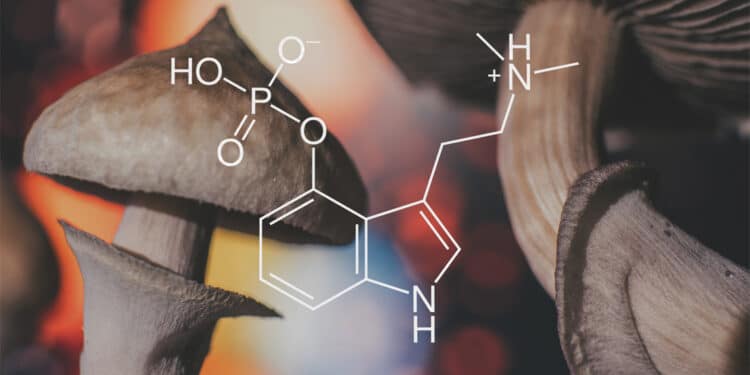
First let's look at what keeps cancer cells alive, then we will come back and examine how the cannabinoids CBD (cannabidiol) and THC (tetrahydrocannabinol) unravels cancer?s aliveness.
In every cell there is a family of interconvertible sphingolipids that specifically manage the life and death of that cell. This profile of factors is called the "Sphingolipid Rheostat." If endogenous ceramide (a signaling metabolite of sphingosine-1-phosphate) is high, then cell death (apoptosis) is imminent. If ceramide is low, the cell is strong in its vitality.
Very simply, when THC connects to the CB1 or CB2 cannabinoid receptor site on the cancer cell, it causes an increase in ceramide synthesis which drives cell death. A normal healthy cell does not produce ceramide in the presence of THC, thus is not affected by the cannabinoid.
The cancer cell dies, not because of cytotoxic chemicals, but because of a tiny little shift in the mitochondria. Within most cells there is a cell nucleus, numerous mitochondria (hundreds to thousands), and various other organelles in the cytoplasm. The purpose of the mitochondria is to produce energy (ATP) for cell use. As ceramide starts to accumulate, turning up the Sphingolipid Rheostat, it increases the mitochondrial membrane pore permeability to cytochrome c, a critical protein in energy synthesis. Cytochrome c is pushed out of the mitochondria, killing the source of energy for the cell.
Ceramide also causes genotoxic stress in the cancer cell nucleus generating a protein called p53, whose job it is to disrupt calcium metabolism in the mitochondria. If this weren't enough, ceramide disrupts the cellular lysosome, the cell's digestive system that provides nutrients for all cell functions. Ceramide, and other sphingolipids, actively inhibit pro-survival pathways in the cell leaving no possibility at all of cancer cell survival.
The key to this process is the accumulation of ceramide in the system. This means taking therapeutic amounts of CBD and THC, steadily, over a period of time, keeping metabolic pressure on this cancer cell death pathway.
How did this pathway come to be? Why is it that the body can take a simple plant enzyme and use it for profound healing in many different physiological systems? This endocannabinoid system exists in all animal life, just waiting for its matched exocannabinoid activator.
This is interesting. Our own endocannabinoid system covers all cells and nerves; it is the messenger of information flowing between our immune system and the central nervous system (CNS). It is responsible for neuroprotection, and micro-manages the immune system. This is the primary control system that maintains homeostasis; our well being.
How does the work get done at the cellular level, and where does the body make the endocannabinoids? Here we see that endocannabinoids have their origin in nerve cells right at the synapse. When the body is compromised through illness or injury it calls insistently to the endocannabinoid system and directs the immune system to bring healing. If these homeostatic systems are weakened, it should be no surprise that exocannabinoids are therapeutic. It helps the body in the most natural way possible.
To see how this works we visualize the cannabinoid as a three dimensional molecule, where one part of the molecule is configured to fit the nerve or immune cell receptor site just like a key in a lock. There are at least two types of cannabinoid receptor sites, CB1 (CNS) and CB2 (immune). In general CB1 activates the CNS messaging system, and CB2 activates the immune system, but it's much more complex than this. Both THC and anandamide activate both receptor sites. Other cannabinoids activate one or the other receptor sites. Among the strains of Cannabis, C. sativa tends toward the CB1 receptor, and C. indica tends toward CB2. So sativa is more neuroactive, and indica is more immunoactive. Another factor here is that sativa is dominated by THC cannabinoids, and indica is predominately CBD (cannabidiol).
It is known that THC and CBD are biomimetic to anandamide, that is, the body can use both interchangeably. Thus, when stress, injury, or illness demand more from endogenous anandamide than can be produced by the body, its mimetic exocannabinoids are activated. If the stress is transitory, then the treatment can be transitory. If the demand is sustained, such as in cancer, then treatment needs to provide sustained pressure of the modulating agent on the homeostatic systems.
Typically, CBD gravitates to the densely packed CB2 receptors in the spleen, home to the body's immune system. From there, immune cells seek out and destroy cancer cells. Interestingly, it has been shown that THC and CBD cannabinoids have the ability to kill cancer cells directly without going through immune intermediaries. THC and CBD hijack the lipoxygenase pathway to directly inhibit tumor growth. As a side note, it has been discovered that CBD inhibits anandamide reuptake. Here we see that cannabidiol helps the body preserve its own natural endocannabinoid by inhibiting the enzyme that breaks down anandamide.
This brief survey touches lightly on a few essential concepts. Mostly I would like to leave you with an appreciation that nature has designed the perfect medicine that fits exactly with our own immune system of receptors and signaling metabolites to provide rapid and complete immune response for systemic integrity and metabolic homeostasis.
Biochemist Dennis Hill graduated from the University of Houston and did his Graduate Work at Baylor Medical School. Dennis worked as a Cancer Researcher at the MD Anderson Cancer Center in Houston. When Dennis was diagnosed with advanced stage prostate c
www.cureyourowncancer.org