Meet the scientists who may have found the cure for drug addiction
Keegan Hamilton, BuzzFeed
October 9, 2014
After nearly two decades of research, Dr. Stanley Glick developed a drug with the potential to revolutionize substance abuse treatment. It is called 18-MC (short for 18-methoxycoronaridine) and it is, in essence, a drug to get people off of drugs. Glick meticulously tested it on animals, observing as rats hopelessly strung out on cocaine suddenly lose their desire to get high after a few doses of 18-MC. It has a similar effect on animals addicted to methamphetamine, morphine, alcohol, and nicotine. It even seems to work with sugar, indicating potential as an obesity treatment. But it's not rats that Glick is trying to help, and that's where this gets tricky.
“We hope it’s a paradigm shift in the way substance abuse is treated,” says Steve Hurst, CEO of Savant HWP, the Bay Area biotech startup developing 18-MC.
“But we’re still trying to figure out if it’s OK to give to people in doses that are safe enough to replicate what we see in animal models.”
Naturally, there is cause for skepticism. Although early indications suggest 18-MC is safe, it is related to a naturally occurring substance known to cause severe nausea, intense hallucinations, and other serious side effects. Initial tests on humans haven’t revealed those problems, however, and experts are cautiously hopeful that 18-MC may ultimately allow doctors to prescribe medication that blocks cravings and helps people stay clean.
While a handful of treatments are available to help opiate addicts kick their habits, there are currently no options other than cold turkey for coke, meth, and other addictive stimulants. Glick’s 18-MC is one of several promising new substances to emerge from the rapidly advancing field of anti-addiction science. Glick and Hurst’s competitors include a researcher at Weill Cornell Medical College who has created a vaccine that creates antibodies that he says act
“like little Pac-Men floating around in the blood” gobbling up cocaine in the bloodstream before it ever reaches the brain. Another treatment being developed by a Swiss pharmaceutical company and a researcher in New Zealand regulates dopamine, the pleasure-inducing neurotransmitter associated with cocaine, to reduce cravings and prevent relapse.
Despite desperate demand by millions of suffering addicts and their families, it may still take years to determine if these drugs are safe and effective enough to be sold in the United States. Prohibitive costs and red tape have long hindered the development of all types of medication, but public health officials, legislators, academic researchers, and drug developers interviewed for this story say current Food and Drug Administration policies make it especially difficult for companies to bring anti-addiction drugs to market. The FDA requires drugs like 18-MC to produce absolute abstinence in cocaine users in clinical trials, a standard that many believe is impossibly stringent.
Though still staring down a long path of bureaucratic hurdles, Glick and his peers are closer than they’ve ever been before to developing the first medications that combat cocaine and other stimulants. And, after years of shunning anti-addiction science, pharmaceutical companies have begun to realize the potential profits involved and are showing interest in the emerging field.
"Here’s a compound that is effective for models of opioid addiction, stimulant addiction, alcohol addiction, nicotine addiction, and for obesity," says Dr. John Rotrosen, director of the addiction research program at New York University’s Langone Medical Center. Of 18-MC, he says,
"It all seems too good to be true."
Though he officially retired in June, Stanley Glick still teaches at the graduate school, and his vitality belies his senior citizen status. His roots as a native New Yorker show through as he talks a mile a minute while recounting the path he traveled to develop 18-MC.
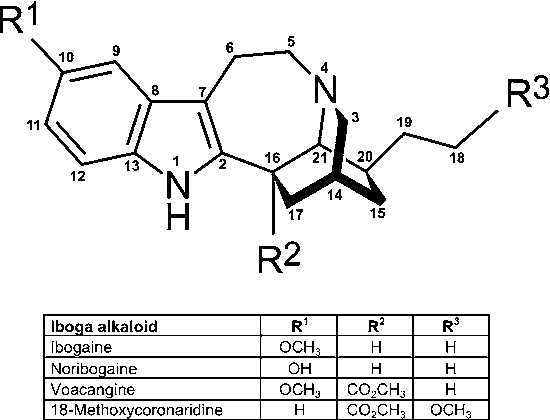
It began one day around 1989 when he received a phone call from a former heroin addict touting a miracle cure for drug addiction. The ex-junkie was named Howard Lotsof, and his purported cure was a substance called ibogaine, a bitter white powder derived from the roots of a plant indigenous to the rainforests of western Central Africa. Ibogaine is something like the African equivalent of peyote or ayahuasca, a potent hallucinogen used to induce spiritual visions during tribal ceremonies.
Glick wasn’t buying it. As both a Ph.D. and medical doctor specializing in substance abuse treatment, he had been studying the effects of addictive drugs on the brain long before Lotsof came calling.
“I’ve gotten a number of calls over the years from people who want me to study something,” Glick says.
“Most of them are just crackpots. But he kept calling back. The more I looked into it, the more my curiosity was piqued.”
Ibogaine is illegal and considered a Schedule I drug in the United States (meaning it officially has a high potential for abuse and no medicinal value), but Lotsof, who died in 2010, was adamant that it eliminated the intense cravings and unpleasant withdrawal symptoms associated with heroin and other opiates. He had obtained a patent for the use of ibogaine in treating addiction, and reportedly had positive results administering it at a clinic in the Netherlands, one of many countries where the drug is legal and still available today.
“Lotsof originally thought if he told the world about this, they would embrace him as a savior and he would rid the world of this terrible scourge of addiction,” Glick says.
“Then he realized there was such a thing as science, the FDA, and controlled trials. He had to get scientists to study it. He called every drug abuse scientist in the country, and, for better or worse, I was the first one who was fool enough to get interested in it.”
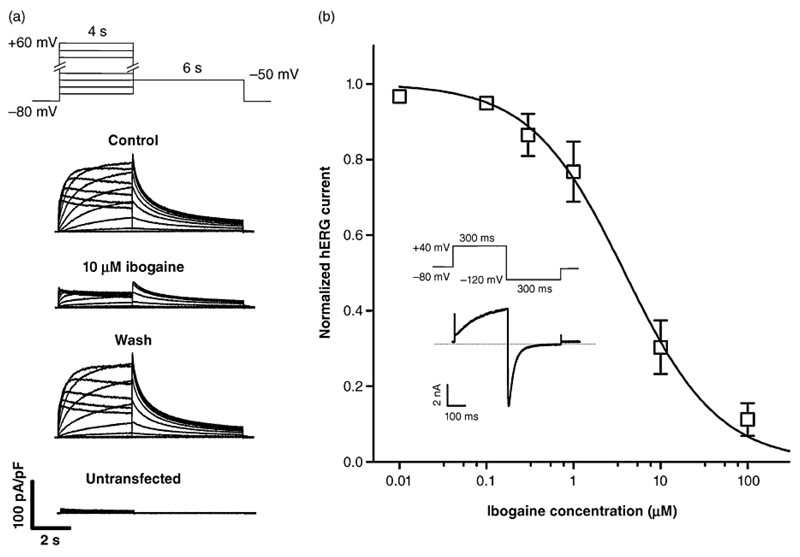
Glick figured a few preliminary tests on rats would debunk Lotsof’s wild claims, but he became intrigued when animals trained to self-administer morphine stopped taking the drug for days and even weeks after being dosed. He set out to find the precise “mechanism of action” in the brain that caused the phenomenon. A few years later, Glick ended up with 18-MC.
The ibogaine research hit a dead end in 1995 when the National Institute on Drug Abuse, the federal agency that funds scientific research on drug abuse, voted to halt the study of ibogaine over concerns the drug causes fatal cardiac issues and possibly brain damage at high doses.
“They just washed their hands of the whole thing,” Glick says.
“It became pretty clear to me there was no way, shape, or form that ibogaine would ever be something that would even be pursued as a legitimate medication in this country.”
A few years prior to the NIDA vote, Glick began collaborating with a chemist at the University of Vermont named Martin Kuehne. Kuehne had experience synthesizing medications for cancer and other diseases, and together they had the idea of tweaking the basic chemical structure of ibogaine to eliminate the side effects while keeping the potent anti-addiction properties. After testing about 60 different compounds — all close chemical cousins of ibogaine — Glick settled on 18-MC.
In simple terms — which Glick often has trouble using — 18-MC blocks the pleasurable effects of cocaine by “dampening the response” to dopamine. Glick pulls up several graphs that show the cocaine intake of addicted rats dropping precipitously after they receive 18-MC.
“What the rat is telling you here is, ‘The drug is getting in, I feel it, but it’s not giving me the kick that it used to,’” Glick says.
“That’s really the essence of how we think 18-MC works. ... No matter what dose of the addictive drug you take, it’s just not giving you the buzz it used to.”
Virtually every addictive drug known to man, from booze to heroin to cocaine, stimulates an area of the brain commonly known as the reward pathway. When a person snorts a line or downs a shot of liquor, it triggers a surge of dopamine in this pathway. Many others have tried unsuccessfully to create drugs that work directly inside the reward pathway by blocking the release of dopamine or preventing it from binding with neurons. Glick’s drug takes a different tact.
According to Glick, 18-MC works on a specific type of nicotinic receptor, an area strongly associated with tobacco addiction and cravings. Most crucially, it also works in an “alternate reward pathway” that indirectly impacts the way neurons in the brain release and absorb dopamine.
“It turned out that in the early ‘80s there was a flurry of studies on this,” Glick says.
“But by the late ‘80s everyone was studying dopamine. We had discovered how rewarding events occur in the brain and everyone had forgotten about this alternate reward pathway. I felt like what happened is we rediscovered the importance of this pathway.”
After Glick made his first discoveries about 18-MC, he set about finding a partner willing to invest in the additional research and development necessary to gain FDA approval for testing in humans. He ended up writing letters to 38 different pharmaceutical companies. Nobody was interested.
“I’d done everything conceivable I could do to try to get some pharmaceutical interest,” Glick says.
“I was on the verge of giving up.”
As Glick soon learned, he was hardly the first addiction researcher to be spurned by big pharma. For a variety of reasons, industry titans have long been reluctant to develop treatments for drug addiction. The main problem, according to several scientists interviewed for this story, is one of perception: Corporations simply don’t want their brands associated with dope fiends, cokeheads, and tweakers.
Dr. Jed Rose, director of the Duke Center for Smoking Cessation and a professor in the Department of Psychiatry and Behavioral Sciences at Duke University Medical Center, says the stigma of drug addiction is so strong that companies have even been reluctant to invest in something as seemingly mainstream as anti-nicotine research. Rose says he has experienced instances where drugs for schizophrenia and Alzheimer's also showed potential as smoking treatments, but no further testing was permitted.
“Over the years I’ve pleaded with companies to allow us to test their agents on smoking,” Rose says.
“Time and time again I was refused. The companies didn’t want to have their image tainted with addiction, even smoking addiction.”
Another issue is a perceived lack of profitability. According to the National Survey on Drug Use and Health, in 2013 an estimated 1.5 million Americans used cocaine, but only a fraction of those could be expected to receive treatment in any given year. Many hardcore users also abuse alcohol, opiates, and other drugs, making pharmacological treatments a dicey proposition in terms of safety and efficacy.
“Pharma thinks drug addiction is not a good enough market,” says Nurulain Zaveri, president and CSO of Astraea Therapeutics, a San Francisco Bay Area startup developing an addiction drug that targets the same set of nicotinic receptors as 18-MC.
“It’s fraught with risk. You’re dealing with high-risk people who have addictions. It’s a disease of the mind. When you’re dealing with drugs that work on the brain, it’s risky business.”
In recent years, however, pharmaceutical companies have gradually come to realize that major money can be made treating addiction. The catalyst for this shift is the drug buprenorphine (commonly sold as the compound Suboxone), an anti-opiate medication that generated $1.5 billion in sales in 2012 — outselling both Viagra and Adderall.
Buprenorphine was introduced in Belgium in 1983, but did not become widely available in the U.S. until 2003. The drug allows addicts to gradually taper down their opiate intake, mimicking heroin in the brain but with more muted effects on the body. The FDA granted the drug "orphan" status, which is intended for products that treat rare diseases. From a business perspective, the appeal of orphan drugs is that they qualify for significant tax credits, and the FDA cannot rescind status after it is granted. Suboxone sales have skyrocketed in conjunction with the recent rise of heroin and painkiller addiction.
NYU's Rotrosen believes pharmaceutical companies have recently become much more receptive to anti-addiction drugs after the stunning success of Suboxone.
“Nobody saw addiction as a profitable area,” he says.
“The fact that buprenorphine has been successful and the fact that addiction is in many ways becoming an everyman’s disease, rather than one for down-and-out junkies, has changed that.”
Perception was initially part of Glick’s problem too. Potentially hallucinogenic miracle cures are a tough sell, no matter how promising the data. The unusual experiments with rats and Miles Davis haven’t always gone over well either. A related experiment landed him on a list of “Most Ridiculous Research on Animals” compiled by In Defense of Animals, a California-based animal rights group.
“I had reporters breathing down my neck,” Glick grumbles.
“It was because they looked at the one paper and didn’t realize it was a series leading up to what we wanted to do with it.”
Two twists of fate helped Glick reverse his fortunes. In 2010, he gave a talk at the prestigious American College of Neuropsychopharmacology Annual Meeting, an event where elite biochemists and neuroscientists convene to discuss the state of their field. He recalls arriving late on a delayed flight the night before his presentation —
“I thought I was half asleep” — but later received unprecedented interest in his project, particularly from NIDA.
“Within a week I started getting a whole bunch of calls from people who were interested,” Glick says.
“All of a sudden they wanted to help me.”
Also in 2010, Glick was approached by Steve Hurst, the founder and CEO of Savant HWP. An attorney with a background in patent law, Hurst has years of experience in the pharmaceutical industry, working previously with groups that developed an inhalable form of insulin and other novel medications, including a clot-busting stroke medicine derived from snake venom. Glick says Hurst
“knows more science than any lawyer I’ve ever met.”
The pair agreed to a partnership, and Hurst added to the equation business savvy and connections that Glick sorely lacks. Personality-wise, the two are polar opposites. While Glick is staid and erudite, Hurst sips a glass of bourbon neat during an interview at the posh Tribeca Grand Hotel in Manhattan and casually riffs on the science of addiction and the failure of the war on drugs.
“We know that addiction is a disease and that ‘Just Say No’ is a delusion,” Hurst says.
“If your brain tells you to go drink, or do cocaine, or shoot heroin — that’s not willpower. This whole notion is a reason I think addiction medicine is such an emerging field. We understand a lot about the disease we didn’t understand 10 years ago.”
With Hurst’s help, in September 2012, Glick secured a $6.5 million grant from NIDA to prepare 18-MC for clinical trials in humans. After more than a year of exhaustive toxicology analysis and other procedures to prove the drug is unlikely to cause serious harm in people, the first limited trial was tentatively scheduled to begin earlier this year on seven healthy volunteers at a facility in Kansas.
“As you can imagine, it’s very, very difficult for addicts to achieve drug abstinence,” says Dr. Ivan Montoya, a deputy director at NIDA.
“We are in a dialogue with [the FDA] and trying to see if it’s possible to have a significant drug-use reduction as an outcome measure.”
When a company submits an Investigational New Drug (IND) application to the FDA, the agency has 30 days “to review the IND for safety to assure that research subjects will not be subjected to unreasonable risk.” Exactly 30 days after filing the paperwork, Hurst says he received a call from the FDA informing him that the project was on hold indefinitely pending further review.
“They said basically, ‘We have no info for you as to why, and you'll get a letter within 30 days,'
” Hurst says.
“It was one of the oddest FDA calls I've ever been on.”
FDA spokeswoman Sandy Walsh declined to comment on the status of 18-MC.
“For pending applications, under the law FDA staff are prohibited from discussing the existence of, or status of, any drug application,” Walsh said via email.
“That is confidential information.”
Meanwhile, Glick and Hurst constantly receive email from people pleading for a chance to be among the first crop of 18-MC human guinea pigs. The messages are gut-wrenching. One shared by Glick is from a mother seeking help for her “horribly addicted” 28-year-old disabled daughter.
“Our family has done everything we can think of,” the mother wrote.
“She’s been through inpatient rehab, outpatient treatment, Suboxone and methadone clinics. She wants out of addiction or out of this life.”
Glick says he responds personally to every message, but his replies are a cold comfort at best. He urges them to try a conventional treatment and explains that he and Hurst are working diligently to bring 18-MC to market.
“It just breaks my heart,” Glick says.
“I can’t do much to help them. The really sad part is that they are usually ridiculously grateful because usually they can’t get anybody to even talk to them.”
From 2003 to 2005, 115 addicts at a methadone clinic in West Haven, Connecticut, volunteered for an experimental new treatment. Heroin was their main problem, but 9 out of 10
“considered smoked cocaine their second drug of choice after opioids.” Over the course of 12 weeks, 58 people were injected with a cholera vaccine in addition to receiving their regular dose of methadone.
This was no ordinary vaccine. Researchers from Baylor University had modified the common medicine to fight cocaine. If it worked the way it was intended, the vaccine would make it nearly impossible for people to feel the effects of snorting, smoking, or injecting cocaine. The hope was that the test subjects would lose their taste for the drug when they found out it no longer delivered the high they craved.
Testing showed that 21 people “significantly reduced” their cocaine use, but the rest struggled to abstain from use or fell back into their old ways. A four-week follow-up period revealed little in the way of overall improvement in the group. The vaccine was considered a failure.
“We need improved vaccines and boosters,” the researchers concluded in a paper published in 2009.
Fast-forward five years, and a new and improved cocaine vaccine is on the eve of undergoing a similar trial. Dr. Ronald Crystal of Weill Cornell Medical College is at roughly the same point in the drug development process as Glick and Hurst. Crystal has created a cocaine vaccine that is linked to adenovirus, a cause of the common cold. The idea is that the human body produces much stronger natural response to colds than it does for cholera, meaning the cocaine-fighting component of this new vaccine should be more powerful than before.
“Let’s say you go on the subway and someone sneezes with a common cold,” Crystal explains.
“You may get the cold, but your body will respond to the adenovirus and produce antibodies. The adenovirus is very immunogenic. It evokes very high levels of antibodies against itself. That’s what we’re taking advantage of.”
Crystal has tested his vaccine extensively in mice, rats, and primates, all with promising results. He is in the final stages of safety analysis, and aims to have the vaccine tested in humans by the end of the year. He is skeptical of 18-MC, noting that similar drugs that have attempted to regulate dopamine production inside the brain have caused harmful side effects or been proven ineffective.
“This is a different approach,” Crystal says.
"We’re working outside the brain and developing a shield to prevent the cocaine from reaching the brain.”
But the vaccine is hardly a sure thing either. One troubling finding from the study in New Haven was that many users tried to “override” the vaccine by taking huge doses of cocaine. A number of test subjects had as much as 10 times the amount of cocaine in their blood than would typically be expected, posing a serious risk of overdose. Rather than putting people on the road to recovery, the vaccine seemed to provoke even more intense addiction.
Part of the problem may have been that the original trial involved people who were on methadone treatment for heroin addiction. Crystal says for the next round of vaccine trials,
“We would prefer cocaine-specific individuals, but that doesn’t mean we won’t accept others.”
At NIDA, which has exclusively funded Crystal’s research, Deputy Director Dr. Ivan Montoya says if the cocaine vaccine is ever approved, it
“most likely will be for people who are motivated, with ways of controlling for potential overdoses.” That might mean offering the vaccine only to people who have already shown the ability to stay clean for a few months or weeks — not exactly the neediest group.
Crystal remains optimistic that the more potent vaccine, perhaps combined with booster shots, won’t have the same issues as its predecessor. There’s also the potential to combine the vaccine with enzymes — the molecules in the body responsible for metabolism — to more effectively break down cocaine in the bloodstream. Montoya notes that an Israeli company called Teva Pharmaceuticals has
“developed an enzyme that is 1,000 times more efficient than the natural enzyme that breaks down cocaine,” but it has not yet been approved by the FDA.
Although the vaccine is technically competing with 18-MC, Glick says he hopes the rival treatment turns out to be safe and effective. His concern, however, is that even if the improved vaccine totally blocks the effects of cocaine, addicts will end up substituting other stimulants, such as meth, to achieve a similar high.
“I have my doubts,” Glick says of Crystal’s vaccine.
“If all it does is block the drug from reaching the brain, it doesn’t address the craving or underlying cause of addiction.”
Of course, eliminating cravings is much easier said than done. Scientists know exactly how cocaine and other drugs work once they reach the brain, but relatively little is known about craving and relapse. Glick and others are banking on the idea that indirectly regulating the way brain releases and absorbs dopamine in the reward pathway is the key to solving the riddle.
At the University of Canterbury in New Zealand, Dr. Juan Canales is collaborating with the Swiss pharmaceutical giant Roche to study how certain types of receptors in the brain can be used to modulate dopamine in the reward pathway. Canales focuses on trace amine receptors, which he says
“give us the opportunity to regulate dopamine function in different stages of the addiction cycle.”
Like Glick, Canales devised ways to study relapse in cocaine-addicted rats. By working with trace amine receptors, rats that were once addicted to cocaine stopped self-administering the drug, even after they were given a little taste to remind them of the high. Canales says
"The experiment mimics human addicts who fall hard off the wagon after even the slightest exposure to their drug of choice."
“A cigarette for smokers, a drink for alcoholics, or a little bit of cocaine — that little bit of drug acts as a reminder and they relapse,” Canales says.
“In that situation we’ve blocked relapse. We are able to indirectly modulate dopamine concentrations within a very narrow margin, which keeps the dopamine system in check, not allowing it to go too high or too low.”
The drawback to interfering with the brain’s dopamine system is that it can often cause serious side effects, including abnormal movements of the face and loss of motor skills. Both Glick and Canales have found nothing in their animal research that suggests their drugs will have similar problems, but there’s only way to find out for sure if they’re wrong: testing on real human beings.
When Glick came up with the idea to play a Miles Davis song to rats on cocaine, he wasn’t really considering how ridiculous it might look to the rest of the world. He simply wanted to test whether 18-MC could effectively block cravings for cocaine. And, although he is a jazz fanatic with pictures of Louis Armstrong decorating his office, he claims the choice of the song “Four” had nothing to do with his — or the rats’ — taste in music.
“The reason I chose that song is it has a very limited range of pitches,” Glick explains.
“It’s very recognizable and it’s very repetitive. It doesn’t vary enough so that it arouses the juices. It’s almost monotonous.”
Glick published his findings from the study in 2012, and the results are both impressive and intriguing for what they reveal about 18-MC’s apparent power to make cravings vanish. Glick concluded that 18-MC “blocked cue-induced reinstatement,” which means the addicted rats no longer had any interest in getting high, even when they heard the Miles Davis song. He also speculated that nicotinic receptors — the parts of the brain impacted by his drug —
“may be involved in the mechanism of craving, and that 18-MC may help prevent relapse to drug addiction in humans.”
In July, after a lengthy back-and-forth with the FDA, Hurst convinced the agency to lift the “clinical hold” on 18-MC, clearing the way for human trials to eventually begin in the United States. At the same time, a separate round of trials are already underway in Brazil, where 18-MC holds appeal not only as an addiction treatment but also for leishmaniasis, a nasty parasitic disease that is common in tropical climates. By pure coincidence, 18-MC shows promise as a treatment for both maladies.
The upshot of 18-MC’s dual purpose is that leishmaniasis potentially qualifies as an orphan disease under FDA regulations. That means 18-MC might be eligible for the same tax breaks and fast-track status that led to the blockbuster success of heroin treatment Suboxone.
In a Sept. 23 press release, Savant announced the preliminary results of the first
“double-blind, placebo-controlled human safety study” of 18-MC. The drug was reportedly
“well tolerated by healthy volunteers.” Hurst noted that 18-MC appears to have none of the harmful side effects of ibogaine, and said a peer-reviewed academic article with additional details is forthcoming.
Even if 18-MC ultimately proves ineffective, Hurst says the company can still fall back on the dozens of related compounds created years ago by Glick and Kuehne. From a business perspective, Savant might not have that kind of time. Rival companies are developing similar drugs that work on nicotinic receptors, and a Florida group is in the advanced stages of testing an anti-opiate drug that uses noribogaine — a naturally occurring metabolite of ibogaine — as the key component.
Yet as of right now, no major pharmaceutical companies are interested in developing 18-MC. The problem is apparently not with the safety of the drug. At NIDA, Montoya says
“All the preclinical studies that have been done so far seemed to indicate 18-MC is safe to be administered to humans,” and,
“if there are problems, they will be tolerable side effects — it will not be lethal side effects.”
The risks, rather, are regulatory and financial. Even if 18-MC helps a significant percentage of patients reduce their cocaine intake dramatically during a clinical trial, it’s still possible that the FDA would refuse to make the drug available in the United States. The agency mandates that anti-addiction drugs result in nothing short of an addict becoming completely abstinent. Companies are naturally reluctant to wager millions of dollars in development costs on the long odds that virtually every addict who uses 18-MC will stay clean.
Walsh, the FDA spokeswoman, responded to questions about the agency’s abstinence standard by sending a commentary on anti-addiction drugs authored by FDA officials and published in 2012 in an academic journal. The gist of the article is that clinical studies on hard-drug addiction should be treated like studies on alcoholism, where six months of no drinking is the gold standard for success.
In March, Sen. Ed Markey, whose home state of Massachusetts has been plagued by heroin and painkiller addiction, issued a joint statement with 37 other members of Congress imploring the FDA to create
“a larger, faster and more predictable pipeline for the approval of new and promising drugs.” Markey followed up with a sternly worded letter to FDA Commissioner Margaret Hamburg demanding answers about the abstinence standard and the state of anti-addiction research.
“I am concerned that even a perceived focus by FDA on treatments that only result in full cessation of drug use (abstinence) limits the engagement of developers/industry on a broader portfolio of treatment options,” Markey wrote.
Walsh declined to comment on the correspondence, and said the FDA
“will review the letter and respond to Senator Markey directly.” Five months later, the FDA replied to Markey's letter, suggesting that labeling could eventually be used to warn that anti-addiction drugs might not be 100% effective in all cases.
"A better relationship between patterns of drug use, and their clinical benefits, would allow us to identify treatments that are effective in helping patients, even if complete abstinence is not achieved," the FDA wrote.
"We need to better understand what patterns of use, if achieved and sustained, translate to clinical benefit, and so serve as a surrogate for the clinical benefit."
While lawmakers and scientists deal with the red tape, cocaine addiction continues to cause significant public health and crime problems. Roughly 34% of federal prisoners locked up on drug charges were sentenced for cocaine or crack, and cocaine is involved in over a third of illicit drug-related emergency room visits.
Experts emphasize that drugs alone probably aren’t going to cure somebody with a serious addiction. The problem runs deeper than just brain chemistry, involving ingrained habits and lifestyle choices.
“In the end, what you want to change is human behavior,” Rotrosen says.
“And it is not necessarily as easy to change somebody's behavior around cocaine as it is overeating or lack of exercise.”
Glick and Hurst are quick to acknowledge that, even in a best-case scenario, 18-MC isn’t likely to be a panacea. It would likely have to be administered over the course of weeks or months along with conventional rehab. But before that happens, it has to earn the FDA’s stamp of approval. And, though the outlook is positive, Hurst cautions there’s still a long way to go before 18-MC is deemed safe and effective enough for American addicts.
“I tell people it’s sort of like a journey through the Himalayas,” Hurst says of the drug development process.
“You reach the top of the mountain in front of you, and you look out and see another mountain range you have to climb over. We’ve gotten up over the first mountain range. There’s at least another one beyond that.”
https://www.buzzfeed.com/keeganhami...aine-addiction?utm_term=.rwmQ0aBVl#.imO7LONRB