I've been reading the following articles:
https://psychotropical.info/clomipramine-potent-snri-anti-depressant/
https://psychotropical.info/tca-intro/
https://psychotropical.info/snri-intro/
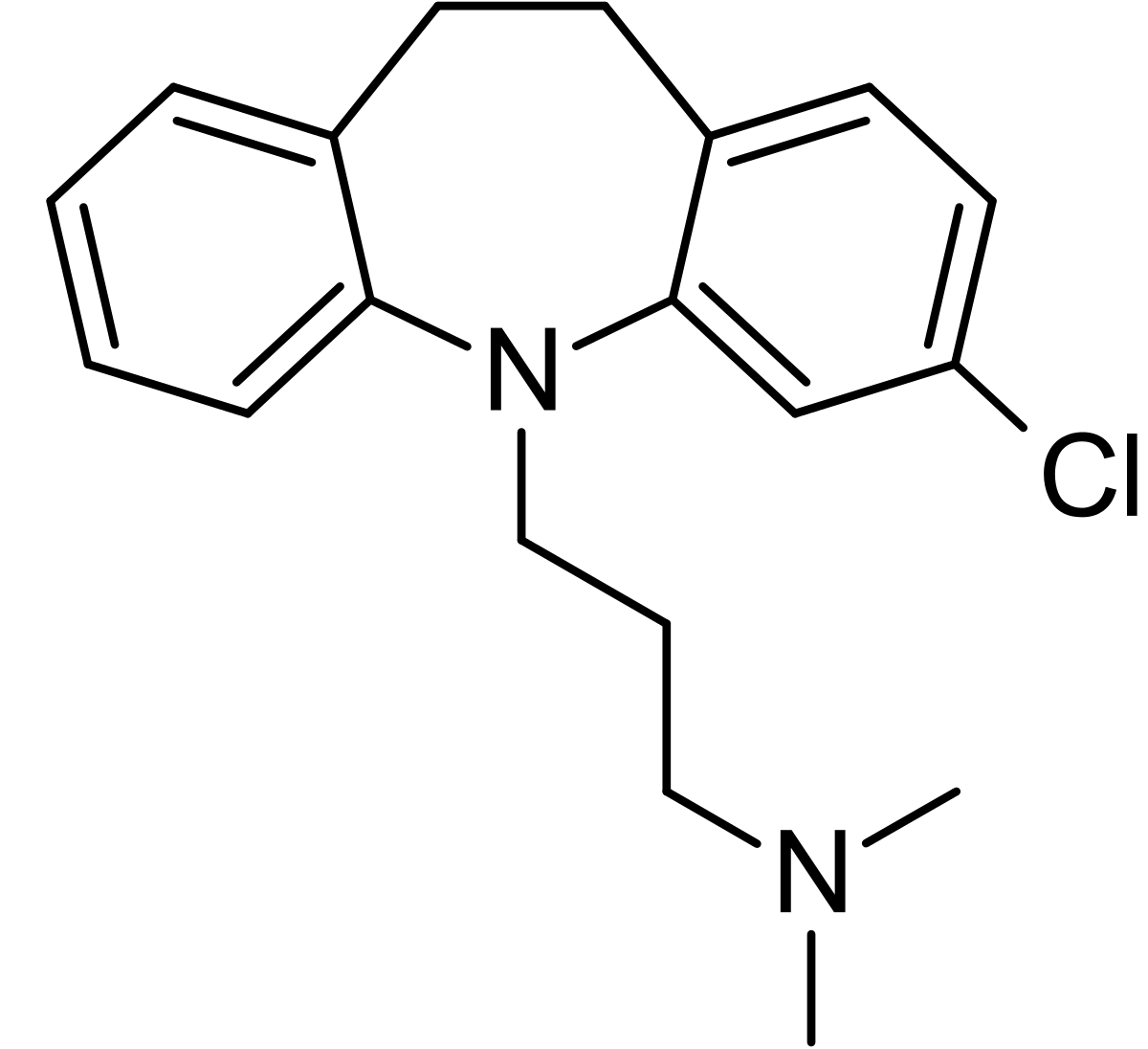
Seems to be a pretty potent drug: SNRI, antagonist of the alpha1-adrenergic receptor, the histamine H1 receptor, the serotonin 5-HT2A, 5-HT2C receptors, the dopamine D1, D2, and D3 receptors, and the muscarinic acetylcholine receptors. It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system; so that speaks for itself.
The reviews on drugs.com and other sites also are quite positive.
The following ranking is interesting: http://slatestarcodex.com/2015/04/30/prescriptions-paradoxes-and-perversities/
These numbers are based on aggregated patient ratings. Top 4 drugs:
# Nardil 1.25
# Parnate 1.23
# Chlomipramine 1.22
# Emsam/selegeline 1.07
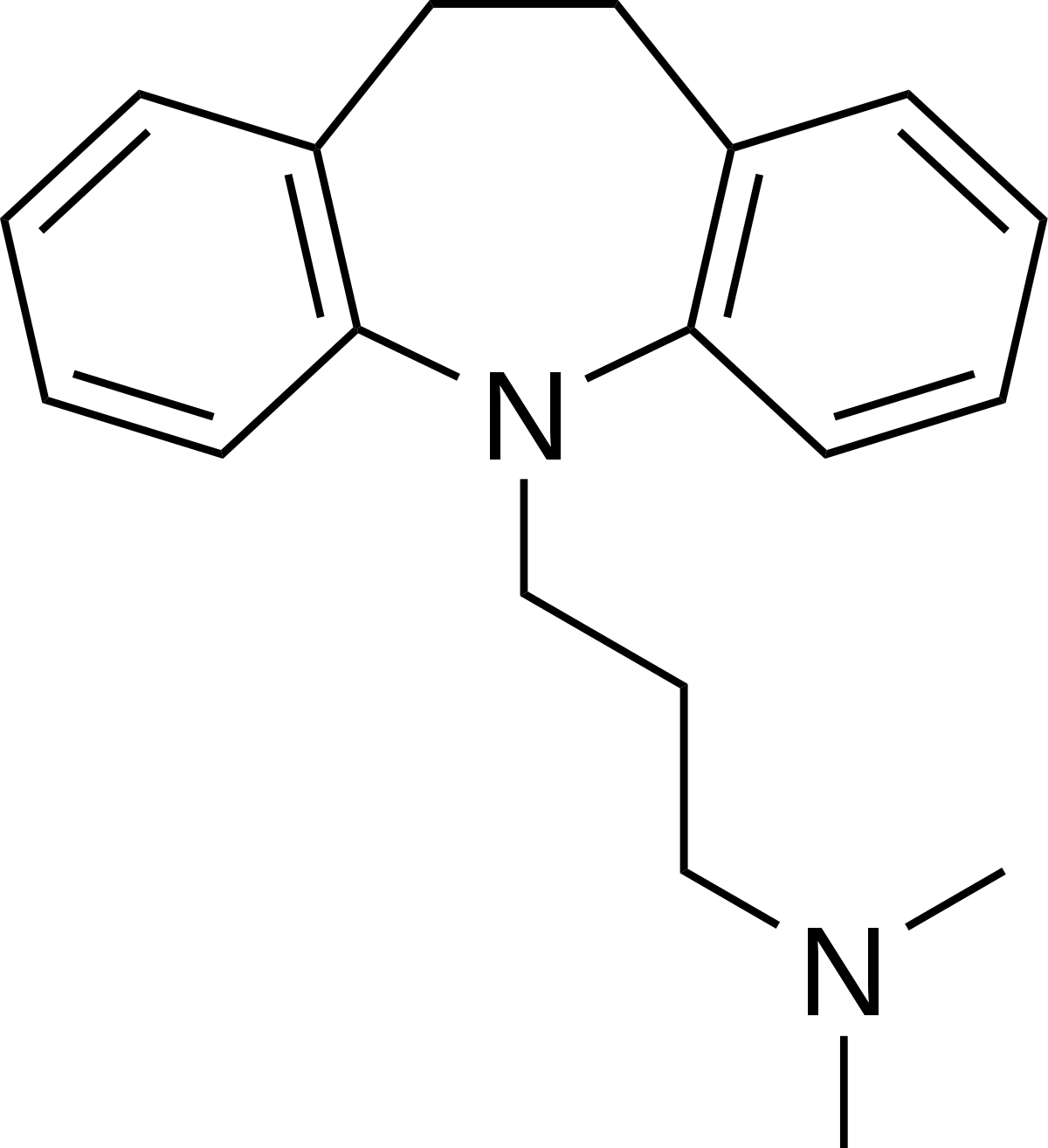
=> Clomipramine roughly on pair with MAOI, followed by Nefazodone (R.I.P) and Imipramine. Imipramine is also a potent SNRI, but lacks the strong 5HT-antagonism compared to Clomipramine. I suppose that's the pharmacological difference which makes Clomipramine superior... ?
Clomipramine exhibits some antagonism of dopamine D1, D2 and D3 receptors... can one expect some clinical & therapeutic benefits from this?
Clomipramine acts as a functional (potent!) inhibitor of acid sphingomyelinase (FIASMA): http://en.wikipedia.org/wiki/FIASMA
Some interesting graphs regarding antidepressant FIASMAs: http://d-nb.info/1011278227/34
Who here has been on Clomipramine and what were your experiences with it?
https://psychotropical.info/clomipramine-potent-snri-anti-depressant/
https://psychotropical.info/tca-intro/
https://psychotropical.info/snri-intro/
Seems to be a pretty potent drug: SNRI, antagonist of the alpha1-adrenergic receptor, the histamine H1 receptor, the serotonin 5-HT2A, 5-HT2C receptors, the dopamine D1, D2, and D3 receptors, and the muscarinic acetylcholine receptors. It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system; so that speaks for itself.
The reviews on drugs.com and other sites also are quite positive.
The following ranking is interesting: http://slatestarcodex.com/2015/04/30/prescriptions-paradoxes-and-perversities/
These numbers are based on aggregated patient ratings. Top 4 drugs:
# Nardil 1.25
# Parnate 1.23
# Chlomipramine 1.22
# Emsam/selegeline 1.07
=> Clomipramine roughly on pair with MAOI, followed by Nefazodone (R.I.P) and Imipramine. Imipramine is also a potent SNRI, but lacks the strong 5HT-antagonism compared to Clomipramine. I suppose that's the pharmacological difference which makes Clomipramine superior... ?
Clomipramine exhibits some antagonism of dopamine D1, D2 and D3 receptors... can one expect some clinical & therapeutic benefits from this?
Clomipramine acts as a functional (potent!) inhibitor of acid sphingomyelinase (FIASMA): http://en.wikipedia.org/wiki/FIASMA
Some interesting graphs regarding antidepressant FIASMAs: http://d-nb.info/1011278227/34
Who here has been on Clomipramine and what were your experiences with it?