Znegative
Bluelight Crew
- Joined
- Apr 15, 2010
- Messages
- 6,019
| ⫸INJECTIONS: I.V. FAQs & Info MEGATHREAD 4⫷ |
| The I.V. Megathread 3 can be found here: https://www.bluelight.org/xf/thread...fo-megathread-faq-iii-vs-i-want-blood.602800/ |
So we've decided to comprise a thread dedicated to Injecting, more specifically people who have had something go wrong and want some information and ask questions. Also included is some information about the injection process and complications that can arise as well as an array of other information to be added.
Intro to Injecting
Injecting drugs into the body gives a 100% Bio-availability, being the most efficient way of introducing and getting high from a drug. Though via the IV route the filtering and delaying mechanisms that protect us when otherwise absorbed via the gastro-intestinal tract, lungs or skin etc are bypassed.
It’s believed that injecting is associated with increased levels of drug dependence and increased risk to health form . A few examples
- blood-borne viruses;
- bacterial infections;
- fungal infections;
- damage to the circulatory system; and
- increased likelihood of overdose.
- Abscesses
- Loss of limbs
- Scarring
- Loss of veins
Correct IV technique
Irreversible damage is likely to occur when there is
repeated use of the same injecting site;
poor technique;
injection with blunt needles;
injection with needles that are too large; and
injection of irritant substances.
poor hygeine involved
Some instructions to follow while shooting up
- washing hands, and cleaning the injection site with soap and water, or an alcohol swab;
- preparing drugs for personal use in your own space, and using equipment that has not been used by anyone else;
- choosing the smallest possible bore and length needle for the site;
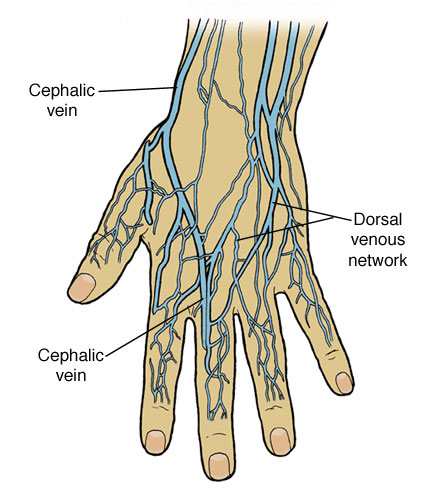
- selecting a suitable vein, and introducing the needle by carefully sliding it under the skin, at a shallow angle and with the bevel up, and then into the vein;
- injecting with the blood flow, i.e. towards the heart;
- pulling back the plunger to identify that the needle is in a vein - a small amount of dark red venous blood should trickle into the syringe. If a tourniquet is used it should be loosened once you have drawn blood back into the syringe;
- injecting slowly to reduce the likelihood of drugs leaking around the needle into the tissues surrounding the vein and damaging the vein;
- injecting the hit in two halves with a short break (a few seconds) between will reduce the overdose risk;
- not jacking back blood and ‘flushing’ after a shot - as this can significantly increase damage to the vein;
- removing the needle slowly and carefully;
- applying pressure to the site with a blood proof pad, cotton wool or tissue (bruising is caused by bleeding into the surrounding tissue. Immediate firm pressure will limit the amount of bruising caused); and
- safely disposing of used injecting equipment, and whatever has been used to stop bleeding.


Differences between arteries and veins
General differences between arteries and veins have been summarised below (adapted from Aldridge & Cranfield 1993).
Arteries
- carry blood away from the heart;
- carry oxygen-rich blood
- (except between the right side of the heart and the lungs);
- hold bright red blood;
- blood at high pressure;
- bleed profusely - spurt blood;
- served by many nerves;
- thick walls;
- very elastic/muscular;
- no valves;
- less numerous;
- recognisable pulse; and
- mostly deep.
Veins
- carry blood towards the heart;
- carry oxygen-depleted blood
- (except between the lungs and the left side of the heart);
- hold dark red blood;
- blood at low pressure;
- do not bleed profusely - ooze blood;
- served by few nerves;
- thin walls;
- not elastic/muscular;
- valves;
- more numerous;
- no pulse; and
- deep and superficial.
Consequences of blocking arteries and veins
There is only one arterial route to each area of tissue in our bodies. If an artery is blocked for any length of time, all the tissue it supplies die.
Venous blood return tends to be more adaptable: veins form a complex network with many junctions. If a vein becomes blocked, blood can find its way through a smaller vessel further back down the system. It is when these smaller vessels become overloaded with blood that swelling occurs in the hands or feet.
Collateral circulation
When a vein becomes thrombosed or obstructed, blood can no longer flow through it to return to the heart. The blood will therefore take an alternative route, using other smaller blood vessels to get around the blockage.
This diversionary circulatory route is called ‘collateral circulation.’
When most of the veins have become obstructed, this process may result in the appearance of ‘new’ superficial veins on or near the skin surface. Injectors should be discouraged from attempting to use these veins, as they are likely to be small veins that have become engorged by the necessity for them to carry more blood.
They will therefore be under greater pressure than normal, so that injecting into them carries a greater risk of damage to the vein. The usual consequence of injecting into such veins is that within a few injections the vein becomes damaged and is no longer viable.
If the remaining veins are also damaged, then the return of venous blood from the affected limb is likely to be even more severely restricted. This will lead to slower blood flow out of the arm and lead to the limb becoming swollen and blue. The consequences of this are discussed below under ‘Long term consequences of substantial vein damage.’
Arterial injection
All drug injectors should be warned that they should never inject into a blood vessel in which they can feel a pulse.
Although most arterial injections are accidental, occasionally people attempt arterial injection deliberately. The practice of deliberate arterial injection should be strongly discouraged.
For those who hit an artery by mistake or otherwise, advice should be to:
- immediately withdraw the needle - do not complete the injection;
- put strong pressure on the site for at least 15 minutes;
- raise the affected limb if possible; and
- seek medical advice.
Arterial injection can sometimes cause weakening of the artery wall (pseudoaneurysm) or fungal infection of the artery wall (mycotic aneurysm). Both conditions can lead to life-threatening arterial bleeding.
Thrombosis
Blood clots form when there is turbulence in the flow. Damage to, or inflammation of, the lining of the vein (figure 8.1) can trigger clotting of the blood at the site of the damage (figure 8.2).
These clots stick to the lining of the vein, and are known as thromboses. The clots themselves cause turbulence and this, in turn, can cause further clotting (figure 8.3).
A blood clot inside a vein does the same things as a blood clot on the surface - it hardens and turns to scar tissue that shrinks and pulls the edges together (figure 8.4).

It is this pulling together of the edges that makes veins ‘collapse.’
Veins that have collapsed in this way do not ‘unblock’ - the blood has to find another way back to the heart.
Vein blockage and collapse
Veins may become temporarily blocked if the internal lining of the vein swells in response to repeated injury or irritation. This may be caused by the needle, by the substance injected, or both. Once the swelling subsides the circulation will often become re-established.
Smaller veins may block as a consequence of too much suction being used when pulling back against the plunger of the syringe to check that the needle is in the vein. This will pull the sides of the vein together and (especially if they are inflamed) the sides of the vein may stick together, causing the vein to block. Removing the needle too quickly after injecting can have a similar effect.
Permanent vein collapse (Figure 8) occurs as a consequence of:
- long-term injecting;
- repeated injections, especially with blunt needles;
- poor injecting technique; and
- injecting of substances which irritate the veins.
Long-term consequences of substantial vein damage
When the flow of blood through the limbs has been severely affected, there are a number of problems that can arise. These include:
.
- ulcers;
- local infection; and
- gangrene
Ulcers
One possible result of serious deterioration of circulation can be painful areas of broken skin known as ulcers.
Ulcers form when the skin is knocked or scratched (or injected into) and the surface is broken. The slow flow of blood means that the cells cannot reproduce quickly enough to heal the wound. The resulting moist and painful wound can take years to heal, and can be compounded by infection.
Factors affecting healing
* diet and nutrition;
* stress;
* poor accommodation; and
* drug and alcohol use.
Treatment of ulcers
Unless a NSP is specifically set up to provide primary health care to clients, the client should be referred to either their general practitioner or an A&E department for assessment and treatment.
Ulcers take many months to heal and may require frequent attendance for treatment. There are strong arguments for advocating that these and other health care needs will best be met within drug treatment and NSP services, because:
- users of drug treatment agencies may not attend if referred to other agencies;
- drug users may tend to believe health problems are to be expected and therefore do little about them; and
- they are less likely to receive discriminatory treatment.
Local infections
As well as risks of systemic infections such as hepatitis and HIV, injecting carries the risk of introducing bacterial and fungal infections to the tissue surrounding the injection site.
Often local infections are caused by bacteria which live harmlessly on the skin being picked up by the needle and forced below the skin where they multiply.
The risks of local infection will be increased by:
- sharing of needles and syringes, and injecting paraphernalia;
- reuse of unsterile injecting equipment (including filters);
- the use of non-pharmaceutical medication;
- unhygienic preparation of drugs; and
- poor personal hygiene.
Providing injectors with an understanding of the ways in which infection may be introduced is crucial. Ideally, they should be aware of the risks they may be exposed to and how to reduce them.
Local infections include abscesses, phlebitis, and cellulitis.
Abscesses
An infected abscess is a localised collection of pus that is encapsulated within inflamed tissue (Figure 9). It can be caused by a wide range of bacterial and fungal infections. An abscess is different from cellulitis in that it has a defined edge and shape.

An abscess is characterised by:
* raised skin surface;
* localised heat;
* tenderness and pain;
* redness of the skin (in white people);
* pus formation; and
* a foul smell if it has begun to discharge.
People with abscesses should be referred for medical advice and treatment. The abscess will require antibiotic treatment and/or lancing to release the pus.
Injectors should be told never to try to lance or puncture abscesses themselves. This can spread infection and without appropriate antibiotic cover they can quickly develop septicaemia (blood poisoning). They should be encouraged to alternate injecting sites as this will lessen the risk of localised inflammation, infection and abscess formation.
Phlebitis
Phlebitis is irritation of the smooth inner lining of a vein (tunica intima). The roughening of the vein lining can encourage the formation of clots.
The vein is reddened or inflamed and can sometimes be felt as a thick cord beneath the skin.
Phlebitis can occur as a result of:
* injecting irritant substances (such as benzos, pills, etc.);
* poor injecting technique;
* infection; and
* accidental injury (i.e. knocks or blows).
An important complication of phlebitis is deep vein thrombosis (DVT) leading to pulmonary embolism.
If phlebitis is suspected the person should be referred for immediate medical advice. Treatment includes resting and raising the limb, antibiotics and anti-inflammatory drugs.
Cellulitis
Cellulitis refers to a painful spreading inflammation of the skin, which appears red and swollen with fluid (this is known as oedema).
Cellulitis can occur as a result of:
* irritant substances lodged in body tissues; and
* serious infection.
Where cellulitis is suspected the client should be referred for immediate medical advice. Treatment includes resting and raising the affected limb, and treatment with antibiotics and anti-inflammatory drugs.
Advice for people who have had cellulitis would include the following measures to prevent reinfection:
* using sterile injecting equipment;
* using sterile water where available and discussing alternatives where it is not;
* avoiding the injection of irritant or heavily adulterated drugs; and
* removing rings prior to injecting if injecting in the hands.
Gangrene
Gangrene is the death of body tissue caused by impaired or absent blood supply. Gangrene can occur as a result of arterial or serious venous damage.
The effect of gangrene can be disastrous, leading to loss of limbs. It can also cause the products of tissue breakdown to enter the bloodstream causing blood poisoning and threatening life.
Arterial damage
Gangrene as a result of arterial damage occurs when an artery is injected into instead of a vein. Often this is as a result of injecting irritant drugs (such as benzos, pills, etc.) into the femoral artery rather than the femoral vein. However, it can occur when people inject into the smaller arteries in the arm.
Gangrene as a result of injecting into an artery can occur in the following ways:
* the artery can go into spasm and interrupt the supply of oxygenated blood to the tissues;
* the injected substance can block the artery,
* interrupting the blood supply to the tissues; and
* small particles of the injected substance
* (micro-emboli) can be transported into and block the capillaries in the tissue - causing their breakdown.
Venous damage
Gangrene following venous damage may be slower to develop, and results when damage to the veins is such that the return of venous blood from the affected limb is no longer adequate; blood gets into the tissues at a faster rate than it can get out. In the end the reduced flow of blood through the tissues is inadequate to sustain them and they die.
Signs and symptoms
* pain;
* loss of feeling and control in an area of skin;
* swelling and dicolouration of affected limb;
* affected extremities, i.e. fingers or toes;
* affected tissue initially becoming white;
* affected tissue eventually blackening; and
* if untreated, affected tissues dropping off.
Prevention and treatment
Injecting drug users need to be given advice on the following subjects to enable them to prevent gangrene occurring:
* the dangers of arterial injection;
* the signs and symptoms of injecting into arteries;
* first aid treatment following accidental arterial injection; and
* discourage injection of crushed tablets and gel-tabs, especially Temazepam tablets,
Temazepam Gelthix capsules, and Diconal.
In the event of symptoms of gangrene occurring, injectors must be aware that:
* this is a serious complication that will not go away unless they get medical help; and
* they must get urgent medical treatment - if the onset is sudden they should call an ambulance.
Other injection site problems
‘Missed hits’
‘Missed hit’ is a phrase used to describe swelling which appears around an injection site during or immediately after injection. It may be caused by fluid entering the tissue surrounding the vein because the needle has:
* not entered the vein properly;
* entered the vein and slipped out again;
* entered the vein and gone through the opposite wall; and
* entered the vein correctly but excess pressure caused the vein to split.
These problems can be prevented by encouraging injectors to:
* check that the needle is in a vein by gently pulling back on the plunger to see that venous blood enters the syringe;
* always releasing the tourniquet before injecting;
* maintain a steady hand whilst injecting;
* smoke a small amount of heroin before injecting, when in opiate withdrawal (if possible);
* use the smallest possible needle and syringe barrel;
* inject at the correct angle (i.e. in line with the vein); and
* inject the fluid slowly.
Basic steps to take after a missed injection:
Note: Seeing a doctor right away is always the safest route. However, if that is not an option for whatever reason, there are steps you can take yourself.
* Apply a hot compress to the site as soon as possible. Heat causes vasodilation, (dilation of the blood vessels), thus allowing for more blood flow and faster disbursement of the drugs lingering in the tissue surrounding the vein. Massage the area gently with the hot compress for 10-20 minutes.
* Afterwards, apply an icepack to the area for another 10-20 minutes. This will remove the remaining swelling.
* Keep an eye on the injection site. If just a typical missed shot, the hot compress and icepack should help significantly and the swelling/redness should start to dissipate after 24 hours.
* If after 24 hours you notice the site getting worse, you may have an infection and you should go to the doctor or ER immediately.
A ‘missed hit’ will mean that the drug is absorbed much more slowly by the body, so that the effect will be less pronounced. It can also lead to other problems such as abscesses, cellulitis, and cutaneous foreign body granulomas.
‘Lumps and bumps’
Many injectors have various ‘lumps and bumps’ under their skin, and these often cause anxiety.
The vast majority are not serious, and are caused by the mechanisms outlined below. Checking the history of that site for causes such as:
* previous abcesses;
* frequently used veins that have now collapsed;
* previous misses; and
* history of tablet injecting
will give strong indicators of the cause.
However, clients should be advised that if they are worried, or if the lump/bump ever changes (size, colour, mobility) they should seek medical advice.
Scar tissue
The scar tissue filling collapsed veins can remain visible, and feel like there is a ‘bit of string’ under the skin, for many years. Sometimes, there can be hard ‘knots’ under the surface of the skin, at the points where there were valves.
As with scar tissue from injuries we suffered as children that persists into adulthood, so scar tissue below the skin surface caused by injecting injuries can remain as a lifelong reminder.
Old abscesses can also leave lumps of scar tissue that remain for many years. When clients mention a lump under their skin the first question to ask is ‘have you ever had an abcess at that site?’
Very often the answer will be yes, and you can reassure them that the probable cause is scar tissue that filled the infected capsule when the abscess healed.
BLUNT/REUSED NEEDLES PICTURE

Sterile abscess
A sterile abscess occurs as a result of injecting irritant substances such as crushed tablets and possibly as a consequence of a ‘missed hit.’
It will often disperse without treatment but, over time, a granuloma may form around it.
Cutaneous foreign body granuloma
Granulomas are benign growths of scar tissue that are associated primarily with subcutaneous injecting or ‘missed hits,’ where the solution has by accident or design ended up in the surrounding tissue. In such cases a residue may stay for many years, eventually leading to granuloma formation.
Many of the common cutting agents for injectable drugs, such as quinine, mannitol, dextrose and lactose, are not thought to cause foreign body granulomas. However the injection of crushed tablets will increase the risk. The principle filler of the tablet is often hydrogenous magnesium silicate, frequently referred to as ‘chalk’ by users.
It should be noted that ‘successful’ intravenous injection of crushed tablets does not remove the risk of granuloma formation. It simply changes the place that they may be found, to the lungs.
Injecting myths
Strokes from air bubbles
There is a generalised belief amongst injectors and the general population that injecting air is ‘not a good thing.’ Whilst this is true, it tends to be somewhat overstressed in terms of importance when priorities for injecting drug users are being considered. It is possible to observe some injectors taking little or no care about hygiene or cross-infection risks whilst injecting, but exhibiting infinite patience when expelling the minutest of air bubbles from a syringe.
Compared to the size of an air bubble, it takes a gigantic volume of air to cause circulatory problems (the blood would froth in the chambers of the heart). Although it is desirable not to introduce air into the veins, even a few 1 ml syringes completely full of air would be unlikely to cause any problems.
Carefully removing tiny air bubbles from a syringe can be seen as evidence that injectors are concerned about their health and are prepared to act to preserve it. Some injectors simply need more information about more important priorities such as hygiene.
Having a second hit to ‘sort out’ a bad one
Some injectors have expressed a belief that the best way to deal with a ‘dirty hit’ (an acute reaction to injection, characterised by shivering and sweating that is usually self-limiting) is to inject again.
Whatever the cause of the reaction, repeating the procedure could at best make the experience worse, and at worst cause overdose.
Common practices that damage veins
Licking the needle tip
It is not uncommon for injectors to lick the tip of the needle before injecting. While it is understandable that people would want to avoid loss of any of their drug, and on seeing a small drop run down the needle want to lick it this practice will add large numbers of bacteria to the needle, and greatly increase the risk of infections (especially fungal infections such as thrush). The dose of drug in the droplet that is ‘saved’ will be tiny, and as heroin is not effective orally it will make no discernable difference to the ‘hit.’
Licking the injection site
Again, this behaviour is not that uncommon and may be part of an attempt to ‘clean’ the injecting site prior to injection. This should be discouraged as it will increase the risk of infections, as discussed above.
Injectors should be encouraged to include stopping the bleeding with a disposable pad or tissue, and both hand and injection site washing with soap and water to their post-injection routine.
‘Flushing’
‘Flushing,’ ‘booting,’ and ‘kicking’ are terms which refer to drawing blood back into the syringe after the drug solution has been injected, in an attempt to ensure that no drugs are wasted by being left in the hub of the syringe.
As a small amount of the drug solution will be retained in the hub of the syringe (how much depends on the type of needle and syringe being used), it makes sense in terms of maximising the amount of drug getting into the body to do this.
However, the small benefit of this must be weighed against the extra damage that will be done to the vein and the fact that this practice will ensure that the injecting equipment used is heavily contaminated with blood. This makes the transmission of blood-borne viruses much more likely if the equipment is re-used by another person.
Some users claim that the process of booting or flushing intensifies the rush, so that they get more pleasure from injecting by doing it (and accordingly do it several times). There is no pharmacological basis for this belief, and they are likely to greatly increase the amount of local irritation caused by injecting if they flush repeatedly - thus shortening the ‘injecting life’ of the vein.
Alternatives to injecting
Smoking or ‘chasing’
The smoking of commonly injected drugs clearly offers lower risks than injecting, both in terms of viral transmission and risk of overdose.
When compared with injecting, smoking commonly injected drugs will offer:
* no risk of viral transmission;
* a lower risk of overdose;
* lower health risks;
* an alternative for those who are finding venous access difficult; and
* an alternative route of administration whilst injection sites are allowed to rest.
There is a potential value in using carefully thought-through campaigns promoting the smoking of commonly injected drugs.
Snorting
Snorting drugs is usually safer than injecting them in terms of the relative danger of transmission of blood-borne viruses. Viral transmission can occur if straws, etc. are used by two or more people.
As with injecting, it is best for each user to have separate equipment for the snorting of drugs. Prolonged frequent snorting of drugs (especially cocaine) can lead to damage to the mucous membranes in the nose and cause, or exacerbate, sinus problems.
Swallowing
Of the commonly injected drugs, swallowing is most effective for amphetamines, which are often taken in this way, either by mixing the drug in a drink or by ‘bombing’ (wrapping it in a cigarette paper to reduce the unpleasant taste).
If an injector is contemplating using a ‘risky’ substance (eg. what is left on a spoon after filtering), swallowing usually represents the safest way of getting it into the body.
For those using benzodiazepines by injection - often as crushed tablets - taking them by mouth is by far the safer alternative and the effect, although slower to ‘come on,’ will ultimately be much the same.
If heroin is swallowed it gets converted to morphine in the stomach and as a result it becomes roughly half the strength. This fact, coupled with the slow absorption into the blood stream, means that it is unlikely to be thought a viable alternative to sniffing or ‘shafting’ by drug users.
Rectal administration: ‘shafting’, 'plugging', 'topshelving'
The functions of the rectum are to store faeces and reabsorb fluid in order to prevent dehydration. It has an excellent supply of blood in order to carry out this function, and this means that any fluid introduced to the rectum is quickly absorbed.
There may be some cultural resistance to this route of administration from injectors as this is an unusual route of drug administration, although some medications are given as suppositories which use the same absorption process.
It can provide for very rapid uptake of the drug (almost as fast as injecting), although not everyone finds this to be the case. In some opiate users the cause of this may be constipation and absorption of the drug by faeces.
The method is simple: the needle is removed from the syringe (essential!), then the tip of the syringe is inserted into the rectum, and the plunger depressed.
It can be suggested as a route of last resort in the event of not being able to find anywhere to inject which is much better than just sticking the needle in anywhere and injecting into the muscle.
It can also give injectors the ritual of drug preparation without the delay of fruitless attempts to find a vein, and slow absorption when they miss.
This was extracted from http://www.saferinjecting.info/vcbrieftext.html#vc brief intro
It’s a great site, visit it. More to come.
Suggestions? Pics? Anything? Pm one of us or post a suggestion.
Compartment Syndrome
Compartment syndrome is an acute medical problem following injury, surgery or in most cases repetitive and extensive muscle use, in which increased pressure (usually caused by inflammation) within a confined space in the body impairs blood supply. Without prompt surgical treatment, it may lead to nerve damage and muscle death.
Symptoms
* Pain is often reported early and almost universally. The description is usually of severe, deep, constant, and poorly localized and is sometimes described as out of proportion with the injury. The pain is aggravated by stretching the muscle group within the compartment and is not relieved by analgesia up to and including morphine
* Paresthesia (alterated sensation e.g. "pins & needles") in the cutaneous nerves of the affected compartment is another typical sign.
* Paralysis of the limb is usually a late finding. The compartment may feel very tense and firm as well (pressure). In some cases, some find that their feet and even legs fall asleep. This is because compartment syndrome prevents adequate blood flow to the rest of the leg.
* Note that a lack of pulse rarely occurs in patients, as pressures that cause compartment syndrome are often well below arterial pressures and pulse is only affected if the relevant artery is contained within the affected compartment.
* Tense and swollen shiny skin
Treatment
Acute compartment syndrome is a medical emergency requiring immediate surgical treatment known as a fasciotomy to allow the pressure to return to normal.
Subacute compartment syndrome, while not quite as much of an emergency, usually requires urgent surgical treatment similar to acute compartment syndrome.
Source
Endocarditis
Endocarditis is an inflammation of the inner layer of the heart, the endocardium. It usually involves the heart valves (native or prosthetic valves). Other structures which may be involved include the interventricular septum, the chordae tendinae, the mural endocardium, or even on intracardiac devices. Endocarditis is characterized by a prototypic lesion, the vegetation, which is a mass of platelets, fibrin, microcolonies of microorganisms, and scant inflammatory cells. In the subacute form of infective endocarditis, the vegetation may also include a center of granulomatous tissue, which may fibrose or calcify.
There are multiple ways to classify endocarditis. The simplest classification is based on etiology: either infective or non-infective, depending on whether a microorganism is the source of the inflammation.
Injection drug users typically experience right-side infective endocarditis.
Endocarditis can also be classified by the side of the heart affected:
* Patients who inject narcotics intravenously may introduce infection which will travel to the right side of the heart classically affecting the tricuspid valve, and most often caused by S. aureus.
* In other patients without a history of intravenous exposure, endocarditis is more frequently left-sided.
Symptoms
Among patients who do use illicit drugs and have a fever in the emergency room, there is about a 10% to 15% prevalence of endocarditis. This estimate is not substantially changed by whether the doctor believes the patient has a trivial explanation for their fever. Weisse found that 13% of 121 patients had endocarditis. Marantz also found a prevalence of endocarditis of 13% among such patients in the emergency room with fever. Samet found a 6% incidence among 283 such patients, but after excluding patients with initially apparent major illness to explain the fever (including 11 cases of manifest endocarditis), there was a 7% prevalence of endocarditis.
Treatment
Treatment usually involves iv antibiotics based on the microorganism involved, and/or surgical treatment.
Source
2, 3, 4, 5
Last edited by a moderator:

 8(%). I would like to relay the following story and information. Although I am OK and used very sterile techniques I will never repeat and nor should anyone.
8(%). I would like to relay the following story and information. Although I am OK and used very sterile techniques I will never repeat and nor should anyone.