lifeisforliving
Bluelighter
- Joined
- Nov 20, 2004
- Messages
- 2,504
I was doing some research for an essay and came accross this on Pubmed. It states that the axons of serotonergic neurons may regrow if they are destroyed by 5,7-dihydroxytryptamine. (If I read that correctly).
I see that the article was done in 1991, so it may be outdated knowledge.. but my question is that if they are now proven to regrow, and the only "real" brain changes that MDMA is "known" to produce is perhaps degradation of the axons.. not the rest of the cell body... wouldn't this suggest that the "damage" that MDMA could do would be transitory and the brain would recover in time?
I guess the possible "Damage" would be from the axons not growing back to the "right" places, or the axons being partially non-functional.
Right?
I see that the article was done in 1991, so it may be outdated knowledge.. but my question is that if they are now proven to regrow, and the only "real" brain changes that MDMA is "known" to produce is perhaps degradation of the axons.. not the rest of the cell body... wouldn't this suggest that the "damage" that MDMA could do would be transitory and the brain would recover in time?
I guess the possible "Damage" would be from the axons not growing back to the "right" places, or the axons being partially non-functional.
Right?
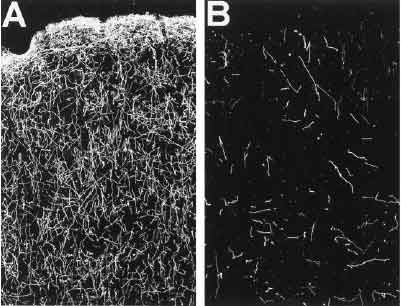
Awakening the sleeping giant: anatomy and plasticity of the brain serotonergic system.
Azmitia EC, Whitaker-Azmitia PM.
Department of Biology, New York University, New York 10003.
The serotonergic neurons of the mammalian brain comprise one of the most expansive chemical systems known. The cell bodies are largely confined to the midline (raphe) region of the brain stem in two general clusters: a superior group that consists of the dorsal raphe nucleus (B-7 and B-6), median raphe nucleus (B-8 and B-5), caudal linear nucleus (rostral B-8), and supralemniscal nucleus (B-9), and an inferior group that consists of nucleus raphe obscurus (B-2), nucleus raphe pallidus (B-1), nucleus raphe magnus (B-3), ventral lateral medulla (B-1/B-3), and the area postrema. The axons from these cells project throughout the neuroaxis from the spinal cord to the olfactory bulb and from the cerebral cortex to the hypothalamus. The development of this giant system begins very early in gestation and is influenced by a variety of growth regulatory factors, including the astroglial protein S-100 beta. Evidence will be presented that the serotonergic system plays a major role in the maturation of the brain by interacting with the 5-HT1A receptors which are most dense during these early developmental periods. The 5-HT1A receptor is located on both neurons and astrocytes, and in the latter cells may serve to stimulate release of S-100 beta. The developmental role of 5-HT appears to become dormant as the brain matures, and during aging and Alzheimer's disease, 5-HT receptors are significantly depressed. However, specific damage to 5-HT fibers in the adult brain by 5,7-dihydroxytryptamine produces a sharp fall in the levels of 5-HT which seems to reactivate the developmental signals in the brain. Not only are the serotonergic fibers encouraged to sprout and expand their territory, but the stimulation of the astrocytic growth factor by a 5-HT1A agonist is reinstated. The ability to recall developmental processes in the adult brain by interrupting the 5-HT fibers may provide important tools for understanding and treating the aged brain.
Publication Types:
* Review
* Review, Tutorial
PMID: 1752858 [PubMed - indexed for MEDLINE]