ScaredFirstTimer
Bluelighter
- Joined
- Dec 15, 2013
- Messages
- 317
Hi, I remember trying to look this up earlier, but after a while of googling, I didn't find a complete answer.
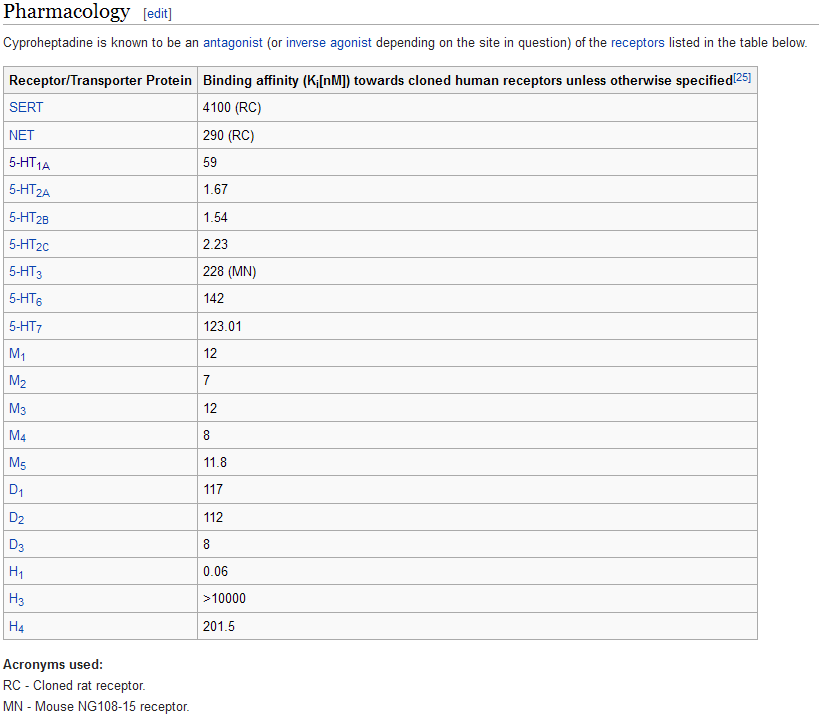
I currently take 5-10mg of Vallargan (alimemazine) sparingly here and there for insomnia. I've also noticed that it's got a pretty effective anxiolytic effect, so I've started taking it earlier in the evening, especially if I'm going out and anxiety is to be expected (currently suffering from MDMA induced anxiety++). Can someone please explain the mechanism of the anxiolytic effect of anti-histamines like this? I remember reading that some anti-histamines are antagonists for several serotonin receptor subtypes as well. Is this the main mechanism by which the anxiolytic effect is achieved?
I currently take 5-10mg of Vallargan (alimemazine) sparingly here and there for insomnia. I've also noticed that it's got a pretty effective anxiolytic effect, so I've started taking it earlier in the evening, especially if I'm going out and anxiety is to be expected (currently suffering from MDMA induced anxiety++). Can someone please explain the mechanism of the anxiolytic effect of anti-histamines like this? I remember reading that some anti-histamines are antagonists for several serotonin receptor subtypes as well. Is this the main mechanism by which the anxiolytic effect is achieved?